LPV/r Drug Interaction Checker
This tool checks for interactions between Lopinavir/Ritonavir (LPV/r) and other medications. Based on the Liverpool HIV Interactions Database, LPV/r interacts with over 1,247 drugs due to CYP3A4 inhibition and enzyme induction effects.
Lopinavir/ritonavir (LPV/r) isn’t just another HIV drug combo. It’s a pharmacological hack - one that changed how we treat viruses, but at a steep cost: a web of dangerous drug interactions that can kill if missed.
Back in 2000, Abbott Laboratories launched Kaletra, a pill combining lopinavir and a tiny dose of ritonavir. The idea? Use ritonavir not to fight HIV, but to block the liver’s main drug-processing enzyme - CYP3A4 - so lopinavir lasts longer in the body. That way, patients could take it just twice a day instead of three times. Simple. Effective. Brilliant.
But here’s what most people don’t realize: ritonavir doesn’t just turn off CYP3A4. It wrecks it. Permanently. And then, on top of that, it turns on other enzymes like CYP1A2 and CYP2C9. This isn’t a switch. It’s a storm.
How Ritonavir Breaks and Fixes Drug Metabolism
Lopinavir, on its own, gets chewed up by CYP3A4 in minutes. Without help, its half-life is under 7 hours. That’s why early HIV patients had to swallow pills every 8 hours - and many didn’t stick with it.
Ritonavir changes that. At just 100mg - 16 times less than lopinavir - it binds to CYP3A4 like glue. It doesn’t just block the enzyme. It destroys its structure. Studies show it forms complexes with the enzyme’s heme group, breaks down the heme itself, and even sticks reactive fragments onto the enzyme’s protein frame. This isn’t temporary inhibition. It’s chemical sabotage.
The result? Lopinavir’s clearance drops to less than 15% of its normal rate. Its half-life stretches to over 12 hours. Dosing becomes manageable. Adherence improves. Lives are saved.
But here’s the catch: CYP3A4 doesn’t just process lopinavir. It handles more than half of all prescription drugs - from statins to painkillers to blood thinners. When you shut it down, those drugs pile up. And when ritonavir turns on other enzymes? Those drugs vanish.
The Interaction Nightmare: 1,247 Drugs at Risk
The Liverpool HIV Interactions Database, updated in July 2023, lists 1,247 drugs that interact with LPV/r. That’s more than any other antiretroviral combo on the market. For comparison, darunavir/cobicistat - a newer booster - has just 892.
Some interactions are deadly. Take rivaroxaban, a blood thinner. Ritonavir boosts its levels so high that bleeding risk spikes. The database says: contraindicated. No exceptions.
Or tacrolimus, used after organ transplants. Ritonavir can make its levels jump 500%. Without a 75% dose reduction, patients risk kidney failure.
Then there’s the flip side. Warfarin? Ritonavir activates CYP2C9, which breaks warfarin down faster. INR levels crash. Blood clots form. You need weekly checks.
Even common stuff like midazolam - used for sedation before surgery - becomes 5 times more potent. Anesthesiologists in Melbourne, Toronto, and Johannesburg now reduce doses by 60-80% for patients on LPV/r. Miss that, and a patient might not wake up.
Hormonal birth control? Ritonavir cuts its effectiveness by half. Women on LPV/r need backup contraception - not just because of HIV risk, but because unintended pregnancy can be dangerous with this regimen.
Why Ritonavir Is Worse Than Cobicistat
When cobicistat came out in 2012, it was supposed to be the cleaner upgrade. It blocks CYP3A4 - same as ritonavir - but doesn’t touch CYP2C9, CYP1A2, or CYP2B6. No induction. No chaos.
That’s why most high-income countries switched. In the U.S., LPV/r use dropped below 5% after 2015. Dolutegravir-based regimens became first-line. Safer. Fewer pills. Fewer interactions.
But ritonavir still has one advantage: cost. In low-income countries, LPV/r costs $68 per person per year. Dolutegravir? $287. PEPFAR programs still rely on it. UNAIDS estimates 28% of first-line HIV regimens in these regions still use LPV/r as of 2022.
That means millions of people are on a drug combo that interacts with nearly half of all commonly prescribed medications. And many of their doctors didn’t train on this.
Real-World Mistakes That Kill
A 2008 study in South Africa showed what happens when you mix LPV/r with rifampicin - a TB drug. Plasma levels of lopinavir dropped 76%. Hepatotoxicity jumped from 11% to 33%. Patients got liver failure. Some died.
Or take voriconazole, an antifungal. Ritonavir both inhibits and induces its metabolism. Levels become unpredictable. The result? Treatment failure - or toxic buildup. The database says: contraindicated.
And then there’s methadone. Ritonavir speeds up its breakdown. Patients on maintenance therapy start feeling withdrawal. Dose increases of 20-33% are needed. But if you don’t know to check, you think they’re relapsing. You don’t adjust. They relapse.
These aren’t edge cases. They’re daily risks in clinics from Kampala to Cape Town.
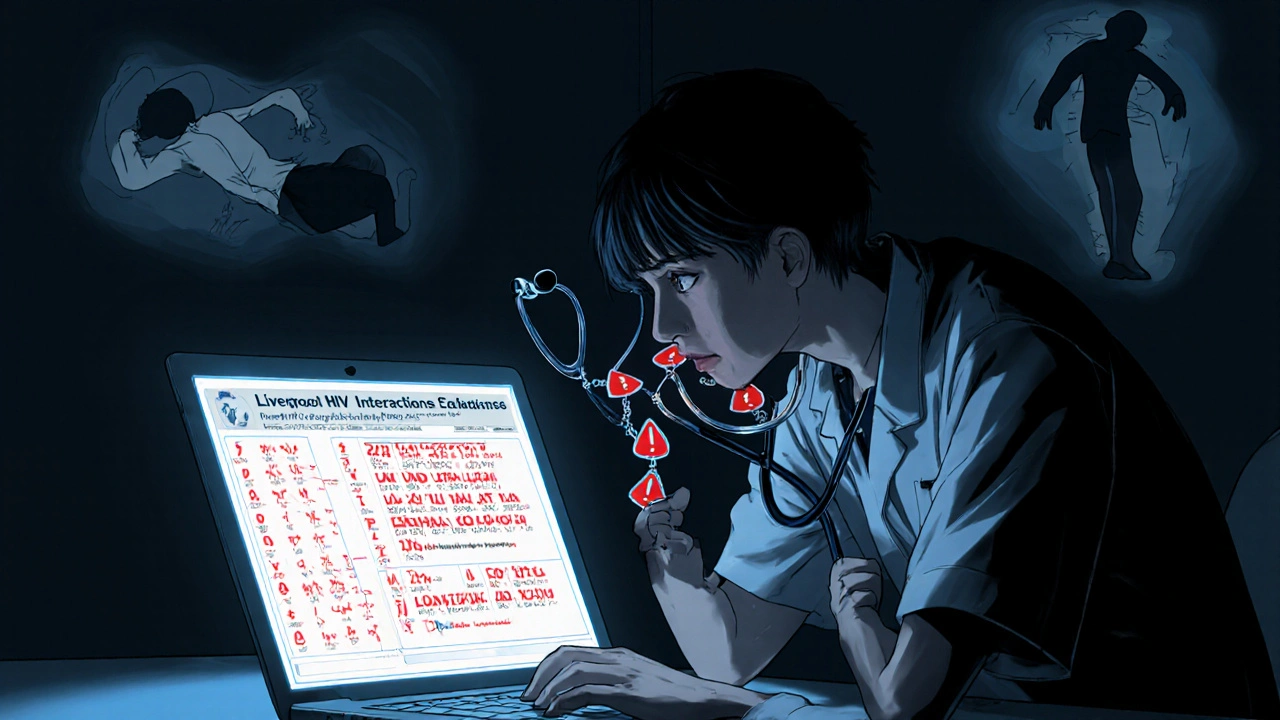
What Clinicians Must Do - And What They Often Skip
Before starting LPV/r, you need 15-20 minutes. Not 5. Not 10. 15-20.
You pull up the Liverpool HIV Interactions Database. You type in every medication the patient is on - including supplements, OTC painkillers, and herbal teas. You flag anything marked ‘Potential Interaction’ - and that’s 48% of all common drugs.
You check for:
- Drugs that need dose reduction (statins, fentanyl, tacrolimus)
- Drugs that need dose increase (methadone, some antidepressants)
- Drugs that are absolutely forbidden (rivaroxaban, ergotamine, alfuzosin)
- Drugs with unpredictable levels (voriconazole, hormonal contraceptives)
You document it. You recheck every time the patient gets a new prescription. You warn them: Don’t start anything new without checking with me.
But most don’t. Why? Because it’s time-consuming. Because they assume the pharmacist will catch it. Because they’ve never seen a bad outcome - yet.
That’s how it starts.
The Future: Decline, But Not Gone
LPV/r is fading. In the U.S., it’s nearly extinct. In Europe, it’s restricted. Even in Africa, dolutegravir is rolling out fast. By 2027, UNAIDS expects LPV/r’s share to drop to 12%.
But it won’t disappear. Not yet. Not while $68 beats $287.
And here’s the irony: ritonavir’s greatest legacy might be Paxlovid. The COVID-19 antiviral uses the exact same trick - 100mg ritonavir boosting nirmatrelvir. But now, the problem is worse. Paxlovid’s ‘rebound’ effect - where symptoms return after treatment - may be linked to ritonavir’s lingering inhibition. The enzyme stays broken for hours after the antiviral is gone. The virus creeps back.
Research is ongoing. NIH is studying how CYP3A5 gene variants affect LPV/r levels. Early data shows people with the CYP3A5 expresser variant clear lopinavir 28% faster. That means some patients are underdosed - even on standard regimens.
So while newer drugs replace LPV/r, the lessons don’t. Ritonavir taught us that boosting isn’t magic. It’s a chemical earthquake. And if you don’t map the fault lines, someone will get crushed.
Bottom Line: Know the Enemy
Lopinavir/ritonavir works. It saved lives. But it’s not a simple pill. It’s a pharmacological landmine.
If you’re prescribing it - or taking it - you need to treat every other drug like a potential bomb. Check every interaction. Document everything. Recheck every time something changes.
Because in this game, the difference between life and death isn’t the HIV viral load. It’s whether you knew that your patient’s new statin could turn into a liver toxin - or that their painkiller could stop their breathing.
That’s the cost of boosting. And it’s not worth it - unless you know exactly what you’re doing.

Aidan McCord-Amasis
November 15, 2025 AT 17:35Katie Baker
November 16, 2025 AT 16:14Adam Dille
November 16, 2025 AT 17:40John Foster
November 18, 2025 AT 08:40Jessica Chambers
November 19, 2025 AT 10:14Ryan Airey
November 20, 2025 AT 14:51Ogonna Igbo
November 21, 2025 AT 03:52Edward Ward
November 21, 2025 AT 21:36Shyamal Spadoni
November 22, 2025 AT 04:36Jonathan Dobey
November 23, 2025 AT 07:31BABA SABKA
November 24, 2025 AT 21:19ASHISH TURAN
November 24, 2025 AT 21:59Andrew Eppich
November 25, 2025 AT 05:04Chris Bryan
November 27, 2025 AT 01:53