When you’re dealing with chronic autoimmune conditions like rheumatoid arthritis, psoriasis, or severe eczema, the goal isn’t just to manage symptoms-it’s to get your life back. For many people, that shift started with the arrival of JAK inhibitors. These aren’t your grandfather’s pills. They’re oral drugs that work inside your cells to quiet down the immune system’s overreaction, and they’ve changed how doctors treat inflammation. But they’re not magic. They come with serious risks, and if you’re on one-or thinking about it-you need to know what to watch for.
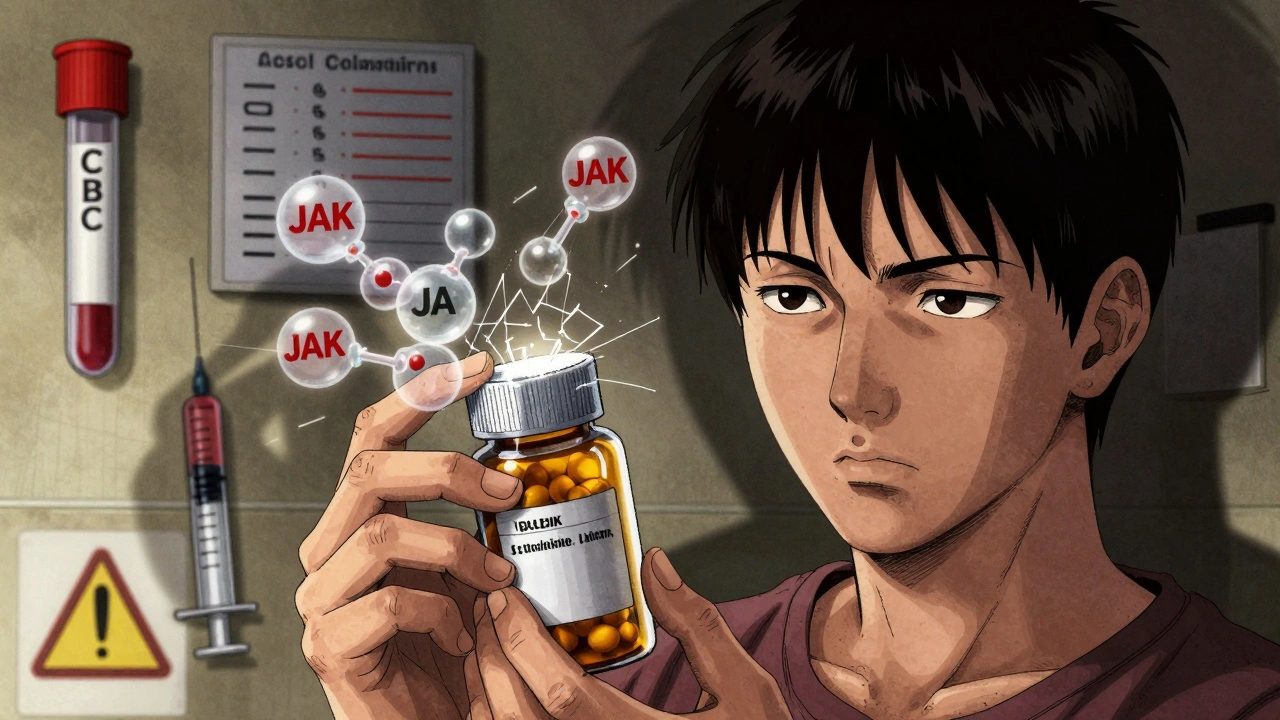
How JAK Inhibitors Actually Work
Unlike biologics that target single proteins like TNF or IL-17, JAK inhibitors go deeper. They block enzymes called Janus kinases-JAK1, JAK2, JAK3, and TYK2-that act like switches inside immune cells. When cytokines (inflammatory signals) bind to receptors on the cell surface, these JAK enzymes turn on a chain reaction that tells the cell to produce more inflammation. JAK inhibitors step in and stop that signal before it even starts.
Think of it like cutting the wires to a loudspeaker instead of just turning down the volume. Drugs like upadacitinib and baricitinib bind tightly to the active part of the JAK enzyme, preventing it from activating STAT proteins. Without those proteins moving into the nucleus, the cell doesn’t crank out inflammatory messengers like IL-6 or interferons. Some newer drugs, like ritlecitinib, even form a permanent bond with the enzyme, making their effect longer-lasting.
This broad action is why one pill can help with both joint swelling and skin rashes. A patient with rheumatoid arthritis and psoriasis might find relief from both with a single daily dose. That’s a big deal when you’ve spent years on multiple injections or creams that barely helped.
Why They’re Popular-And Why Doctors Are Wary
It’s easy to see why patients love them. No needles. No weekly infusions. Just a pill you swallow in the morning. Many report noticeable improvement in joint pain or skin flare-ups within two weeks. A 2023 survey of over 1,200 users found 92% preferred JAK inhibitors over injections. One Reddit user wrote: ‘Abrocitinib cleared my eczema in 10 days.’ Another on HealthUnlocked said baricitinib cut her swollen joints from 18 to 2 in six weeks.
But here’s the catch: the same mechanism that stops inflammation can also lower your body’s defenses. In 2022, the FDA added a black box warning-the strongest possible-to all JAK inhibitors. That means serious risks are proven and well-documented: higher rates of major heart events (like heart attacks and strokes), blood clots, cancer, and severe infections.
The ORAL Surveillance trial followed over 4,000 rheumatoid arthritis patients on tofacitinib versus TNF inhibitors. After five years, those on the JAK inhibitor had a 31% higher risk of major cardiovascular events and a 49% higher chance of developing cancer. That’s not a small number. It’s why the European League Against Rheumatism now says JAK inhibitors shouldn’t be used in patients over 65 with heart disease or a history of cancer.
Who Should-and Shouldn’t-Take Them
Not everyone is a candidate. JAK inhibitors are typically prescribed after methotrexate and one biologic have failed. But even then, you need to pass a safety screen.
Good candidates:
- Patients under 65 with no history of heart disease or stroke
- No personal or strong family history of cancer
- No active infections like tuberculosis or hepatitis B
- Willing to commit to regular blood tests
Avoid if you:
- Have had a blood clot in your legs, lungs, or heart
- Smoke or have high cholesterol you can’t control
- Have had skin cancer, lymphoma, or other cancers in the last five years
- Are pregnant or planning to be
Even if you’re young and healthy, your doctor will check your lipid levels. JAK inhibitors often raise LDL (bad) cholesterol-sometimes by 28 mg/dL or more. That’s not just a number. It’s a ticking clock for heart disease. Statins are often started right away.
What You Need to Monitor-And How Often
Monitoring isn’t optional. It’s the difference between catching a problem early and facing a life-threatening event.
The American College of Rheumatology says you need these tests before starting and regularly after:
- Complete blood count (CBC): Check for low white blood cells or platelets. If lymphocytes drop below 500 cells/μL, you stop the drug.
- Liver enzymes (ALT/AST): If they rise above three times the normal limit, it’s a red flag.
- Lipid panel: LDL over 190 mg/dL means you need a statin. Many patients see increases within the first three months.
- Hemoglobin: If it falls below 8 g/dL, you may need to stop or adjust.
- Tuberculosis screening: Always done before starting. Latent TB can reactivate.
Testing schedule:
- Baseline: Before starting
- Month 1, 3, 6: Every three months for the first year
- After one year: Every six months if stable
Many patients don’t realize how critical this is. One Australian rheumatologist told Australian Prescriber that 45% of patients develop lipid abnormalities within six months-and half of them don’t get statins until it’s too late.
Common Side Effects and What to Do
Side effects aren’t rare-they’re expected. Here’s what most patients experience:
- Herpes zoster (shingles): Occurs in about 23% of users, compared to 3% on biologics. Some need daily antiviral pills like valacyclovir just to prevent outbreaks.
- Upper respiratory infections: Colds, sinus infections, bronchitis. More common than with biologics.
- Nausea and diarrhea: Usually mild and fades after a few weeks.
- Headache and acne: Reported with abrocitinib and upadacitinib.
If you get a fever, persistent cough, or unexplained bruising, call your doctor. Don’t wait. These could signal a serious infection or low blood cell count.
Also, get your shingles vaccine-before you start. The European Medicines Agency recommends it at least four weeks prior. But here’s the problem: 68% of clinics in Europe skip this step because they’re in a rush to start treatment. Don’t be one of them.
What’s New and What’s Coming
The field is moving fast. In June 2024, the FDA approved deuruxolitinib for alopecia areata. It’s the first JAK inhibitor approved specifically for hair loss-and it comes with a mandatory safety program called REMS. That means you can’t get it without enrolling in a tracking system that monitors your blood work and side effects.
Next up: drugs that are more selective. Brepocitinib, a TYK2 inhibitor, is in phase 3 trials and expected to be approved by mid-2025. TYK2 inhibitors may offer the same benefits with fewer side effects because they avoid blocking JAK2, which is linked to blood cell production and cholesterol changes.
Another promising option is ritlecitinib, which binds permanently to JAK3. That means lower doses and possibly fewer off-target effects. Early data shows it works well for alopecia areata and ulcerative colitis.
But here’s the reality check: a 2024 Medscape survey found that 62% of rheumatologists would switch patients to newer biologics if they became available. Why? Because despite the convenience, the safety concerns haven’t gone away. The ORAL Surveillance follow-up in April 2024 confirmed cancer risk stayed elevated even after 8.5 years.
Final Thoughts: Convenience vs. Control
JAK inhibitors are powerful tools. They’ve given people back their lives-faster than any drug before them. But they’re not for everyone. They demand responsibility. You can’t just take the pill and forget about it. You need blood tests. You need to talk to your doctor. You need to know the signs of trouble.
If you’re considering one, ask: ‘What’s my real risk?’ Not just for your disease-but for your heart, your blood, your future. Talk to your rheumatologist about your personal history. Get your labs done. Get vaccinated. Don’t skip the follow-ups.
These drugs aren’t the end of the road. They’re a turning point. And how you handle them will determine whether they help you live longer-or put you at greater risk.

Gareth Storer
December 4, 2025 AT 10:36So let me get this straight - you’re telling me I can swap my weekly needle party for a little white pill that also increases my chance of a heart attack like it’s a loyalty reward? Brilliant. I didn’t know Big Pharma had a ‘Make Life Worse But Make It Convenient’ division. Next they’ll sell us self-driving ambulances with a free subscription to ‘How to Say Goodbye in 140 Characters’.
Pavan Kankala
December 5, 2025 AT 19:57This is all part of the pharmaceutical deep state. JAK inhibitors? More like JAK-TRAP. They want you dependent. They know if you start taking these, you’ll need blood tests forever - and every test is another bill. They’re not curing you. They’re creating a lifetime subscription model. The FDA? Just a rubber stamp for the same guys who sold you cigarettes and opioids. You think they care if you live? They care if you keep paying.
Martyn Stuart
December 7, 2025 AT 17:57Important clarification: JAK inhibitors are not inherently evil - they’re tools. And like any tool, their safety depends on how they’re used. The key is context: age, comorbidities, baseline risk, and, crucially, adherence to monitoring. If you’re under 65, non-smoking, no prior cancer, and you’re doing your monthly CBCs and lipid panels? The risk-benefit ratio can be very favorable. But skipping labs because ‘you feel fine’? That’s not bravery - that’s gambling with your bone marrow. Please, for the love of all that’s medical, get those tests. Your future self will thank you.
Jessica Baydowicz
December 9, 2025 AT 01:41Okay but real talk - I went from crawling to hiking in 3 weeks on upadacitinib. My skin stopped screaming. My joints stopped judging me. Yes, I get blood drawn every 3 months like clockwork. Yes, I’m on a statin now. Yes, I got the shingles shot BEFORE starting. But I’m alive, I’m mobile, and I’m finally sleeping through the night. If this is the price of my life back? I’ll pay it. No regrets. Don’t let fear rob you of your joy - just be smart about it. You’ve got this 💪
Shofner Lehto
December 10, 2025 AT 18:03The ORAL Surveillance data is terrifying but not surprising. What’s worse is how many patients are discharged with a script and zero education. I’ve seen people on JAK inhibitors for 18 months with no lipid panels done. No one told them their LDL shot up to 210. No one warned them about the shingles risk. This isn’t just negligence - it’s systemic. Doctors are overworked. Pharmacies push convenience. Patients assume ‘oral’ means ‘safe.’ It doesn’t. This needs a mandatory patient education module before the first prescription. Not optional. Not a pamphlet. A video, signed acknowledgment, quiz. Something.
Emmanuel Peter
December 11, 2025 AT 13:59So you’re telling me the same drug that fixes my eczema might give me cancer? Cool. So what’s the alternative? Living with skin that looks like a crime scene? I’ll take the statistically improbable death over the daily humiliation. Also, why is everyone acting like this is new? We’ve been doing this with methotrexate for decades - same risks, different mechanism. Just because it’s a pill doesn’t make it less dangerous. But it makes it less visible. And visibility is what scares people. Not the science. The inconvenience.
Ollie Newland
December 12, 2025 AT 03:41One thing nobody talks about: the psychological toll of monitoring. It’s not just the blood draws - it’s the waiting. The anxiety between tests. The ‘what if’ spiral when your platelets dip a little. I’m on baricitinib. I do my labs religiously. But I still Google ‘low lymphocyte count death’ at 2 a.m. The drug gives me my life back - but it also installs a new, permanent roommate: hypervigilance. That’s the hidden cost. No one tells you you’ll become your own lab tech.
Rebecca Braatz
December 13, 2025 AT 23:43Shoutout to everyone doing the work - the ones getting blood drawn, taking statins, reading the fine print, and still showing up for life. You’re not just managing a disease - you’re redefining resilience. And if you’re scared? Good. That means you’re paying attention. Don’t let anyone make you feel crazy for being cautious. This isn’t fear. It’s power. Keep going. You’re not alone.
Michael Feldstein
December 14, 2025 AT 01:48Has anyone here tried brepocitinib yet? I’m in a phase 3 trial for TYK2 inhibition. So far, my lipids are stable, no shingles, and my joints are quiet. The catch? I have to go to the clinic every 4 weeks for bloodwork and a 45-minute intake interview. It’s a hassle - but it feels safer. I’m not saying it’s perfect - but it’s a step toward targeted therapy without nuking your whole immune system. If you’re on a JAK inhibitor and thinking about switching? Talk to your rheum about next-gen options. They’re coming - and they might be worth the wait.
jagdish kumar
December 15, 2025 AT 14:28Life is pain. Pills are just the new crucifix.
Benjamin Sedler
December 16, 2025 AT 00:30Wait - so the FDA says JAK inhibitors cause cancer, but they’re still on the market? That’s not regulation. That’s capitalism with a stethoscope. And now they’re approving deuruxolitinib for hair loss? You’re telling me we’re giving a drug with a black box warning to people who just want their eyebrows back? This isn’t medicine. It’s performance enhancement with a side of mortality risk. Someone’s making a killing. And it’s not the patients.