Two kids come home from school with red, crusty sores around their noses. A few days later, an adult wakes up with a swollen, hot patch on their leg that won’t go away. Both have bacterial skin infections-but they’re not the same. One is impetigo, the other is cellulitis. Mistake one for the other, and you could delay treatment, spread the infection, or even risk serious complications.
What Impetigo Looks Like-and How It Spreads
Impetigo is the most common bacterial skin infection in children, especially between ages 2 and 5. It’s contagious, fast-spreading, and often called "school sores" for a reason. You’ll see it in daycare centers, sports teams, and crowded households.
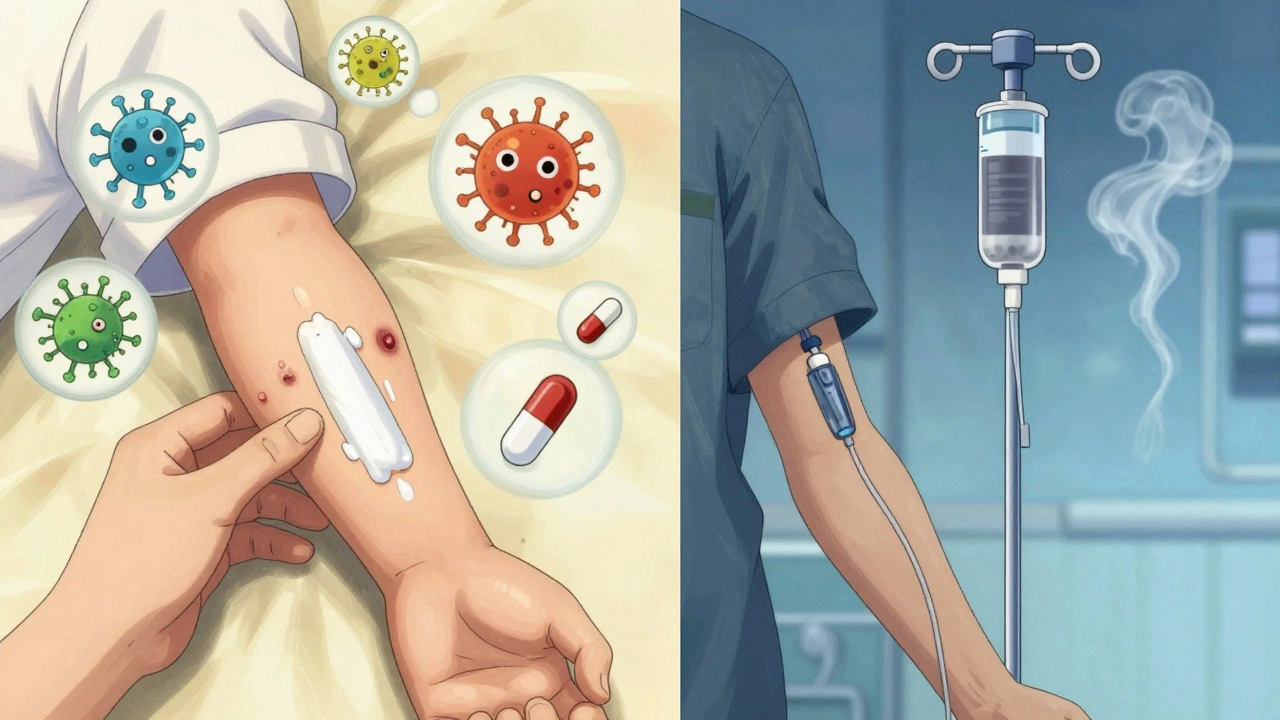
There are two types. The most common-about 70% of cases-is nonbullous impetigo. It starts as small red bumps or blisters, usually around the nose and mouth. Within hours, they burst, ooze, and form a thick, honey-colored crust. It doesn’t hurt much, but it itches. Kids scratch, then spread it to their hands, arms, or legs.
The other type, bullous impetigo, is less common. It shows up as larger, fluid-filled blisters (2-5 cm wide) that look like balloons. They’re fragile and pop easily, leaving behind a raw, red area with a ring-like border. These are more likely to appear on the trunk or diaper area.
What causes it? Mostly Staphylococcus aureus, sometimes Streptococcus pyogenes. These bacteria don’t always need broken skin to get in-they can invade healthy skin. But they love it when there’s a cut, scrape, insect bite, or eczema flare-up. That’s why kids with dry, itchy skin are more likely to get it.
It spreads fast. Touching the sores, sharing towels, or even just being in the same room can pass it along. The CDC says bacterial skin infections like this are among the top 30 reasons people visit doctors. In the U.S., over 14 million outpatient visits each year are for skin and soft tissue infections-and impetigo makes up a big chunk.
What Cellulitis Is-and Why It’s More Dangerous
Cellulitis is deeper. It doesn’t just sit on the surface. It burrows into the dermis and fat layer under the skin. That’s why it’s more serious.
You’ll notice a red, swollen, warm patch that feels tender to the touch. The edges are blurry, not sharp. It often shows up on the lower legs, but it can happen anywhere-arms, face, even around the eyes. Sometimes, fluid leaks out. In severe cases, you might get fever, chills, or feel generally sick.
Unlike impetigo, cellulitis rarely causes crusts or blisters. Instead, the skin looks like it’s been bruised or swollen from an injury-even if there wasn’t one. People often mistake it for a bug bite or a rash at first. That’s dangerous. Delayed treatment can lead to abscesses, sepsis, or even tissue death.
Most cases are caused by Streptococcus bacteria, though Staphylococcus aureus is also common. If the infection comes from a cut or wound, MRSA (methicillin-resistant Staphylococcus aureus) is a growing concern. MRSA doesn’t respond to common antibiotics like amoxicillin or cephalexin. It needs stronger drugs.
People with diabetes, poor circulation, or weakened immune systems are at higher risk. So are older adults and those with leg swelling from heart or vein problems. A 2022 study from Orem Dermatology Center found that the average cellulitis episode lasts 7-10 days with treatment. Without it? It can turn life-threatening in under 48 hours.
Antibiotic Choices: What Works and What Doesn’t
Both infections need antibiotics-but not the same ones. And where you live matters.
For impetigo, if it’s limited to a few spots, topical mupirocin (Bactroban) works well. Studies show it clears up 90% of cases in under a week. But if it’s spread out, or if the child has a fever or swollen lymph nodes, you need oral antibiotics. In the UK and Belgium, flucloxacillin is the go-to. In France, doctors often use amoxicillin-clavulanate or pristinamycin. Why the difference? Resistance patterns. In some areas, staph has grown resistant to flucloxacillin. In others, it still works fine.
For cellulitis, the first-line oral antibiotic is usually amoxicillin-clavulanate or cephalexin. But if MRSA is suspected-like if the person has had recent hospital stays, IV drug use, or lives in a community with high MRSA rates-doctors switch to clindamycin or doxycycline. In severe cases, hospitalization and IV antibiotics like vancomycin are needed.
Here’s a quick comparison:
| Condition | UK & Belgium | France | US Guidelines |
|---|---|---|---|
| Impetigo (mild) | Mupirocin cream | Mupirocin cream | Mupirocin cream |
| Impetigo (widespread) | Flucloxacillin | Amoxicillin-clavulanate or pristinamycin | Cephalexin or dicloxacillin |
| Cellulitis (no MRSA) | Flucloxacillin | Amoxicillin | Cephalexin or amoxicillin-clavulanate |
| Cellulitis (MRSA suspected) | Clindamycin or doxycycline | Clindamycin | Clindamycin or trimethoprim-sulfamethoxazole |
Doctors now avoid using broad-spectrum antibiotics unless they have to. Overuse leads to resistance. That’s why culture and sensitivity tests are recommended for recurrent cases, treatment failures, or if MRSA is suspected. In 65% of those cases, labs now test for resistant strains before prescribing.

When to See a Doctor-And When to Worry
For impetigo: Call your doctor if the sores spread quickly, don’t improve after 3 days of treatment, or if your child has a fever. Don’t wait for it to get worse. It’s contagious. Keep kids home until they’ve been on antibiotics for at least 24 hours.
For cellulitis: Go to urgent care or the ER if you see any of these signs:
- Redness spreading rapidly (more than 1 inch per hour)
- Fever, chills, or nausea
- Severe pain or numbness in the area
- Red streaks leading away from the infection
- Swelling that makes it hard to move a limb
These could mean the infection is entering your bloodstream. That’s sepsis territory. Emergency treatment is needed.
Even if it doesn’t seem bad, don’t try to treat either infection with leftover antibiotics. A wrong drug can make things worse. And never squeeze or pop the sores. That spreads bacteria.
Prevention: Stop It Before It Starts
The best treatment is avoiding infection in the first place.
- Wash hands often-especially after touching sores or bandages.
- Clean and cover cuts, scrapes, or insect bites right away.
- Don’t share towels, clothing, or razors.
- Keep skin moisturized if you have eczema or dry skin.
- If someone in your home has impetigo, wash their bedding and clothes daily in hot water.
- For people with diabetes or poor circulation, check feet and legs daily for redness or breaks in the skin.
Doctors are starting to focus more on "antibiotic stewardship"-using the right drug, at the right dose, for the right time. A 2023 study predicted that within five years, doctors will cut unnecessary antibiotic use by 40% by using faster tests to identify the exact bacteria and its resistance profile.
That means less resistance. Fewer side effects. Better outcomes.
What Happens If You Don’t Treat It?
Impetigo usually clears up on its own-but not without risk. Untreated, it can lead to kidney inflammation (post-streptococcal glomerulonephritis), especially in children. It also spreads like wildfire. One child with impetigo can infect half a classroom in a week.
Cellulitis? It doesn’t wait. Left untreated, it can turn into:
- An abscess (a pocket of pus that needs draining)
- Necrotizing fasciitis (a rare but deadly "flesh-eating" infection)
- Sepsis (body-wide inflammation that can shut down organs)
- Recurrent infections (up to 20% of people get it again within a year)
That’s why early treatment is non-negotiable. Most people feel better within 2-3 days of starting antibiotics. But they must finish the full course-even if the redness is gone. Stopping early lets the toughest bacteria survive and come back stronger.
Can impetigo turn into cellulitis?
Not directly. Impetigo is a surface infection; cellulitis goes deeper. But if you keep scratching impetigo sores, you can create openings for bacteria to enter deeper layers. That’s how cellulitis can start. That’s why it’s critical to treat impetigo early and avoid scratching.
Is impetigo the same as a staph infection?
Impetigo is often caused by staph bacteria, but not all staph infections are impetigo. Staph can cause boils, abscesses, or cellulitis too. Impetigo is just one specific type of staph or strep skin infection that appears as crusty sores.
Can I use over-the-counter antibiotic ointments for impetigo?
Neosporin or similar OTC creams won’t work well for impetigo. They’re designed for minor cuts, not bacterial skin infections caused by staph or strep. Prescription mupirocin is specifically formulated to target those bacteria. Don’t waste time with OTC options-see a doctor.
How long does it take for cellulitis to clear up?
Most people start feeling better in 2-3 days. The redness and swelling usually fade over 7-10 days with oral antibiotics. But if you’re not improving after 48 hours, or if symptoms get worse, you need to go back to your doctor. You might need a different antibiotic or IV treatment.
Are there alternatives to antibiotics for these infections?
No. Antibiotics are the only proven treatment for impetigo and cellulitis. Some people try honey, tea tree oil, or herbal remedies-but there’s no solid evidence they work. In fact, delaying antibiotics can lead to serious complications. Always follow medical advice.
Final Thought: Don’t Guess. Get Tested.
These infections look similar at first glance. But the treatment? Totally different. A rash that seems harmless could be the start of something dangerous. A crusty sore might look like a minor annoyance-but it’s contagious and can spread fast.
The key is knowing when to act. If you’re unsure, see a doctor. Don’t wait. Don’t self-diagnose. And don’t share antibiotics. The right treatment starts with the right diagnosis-and that means letting a professional identify the bacteria behind the redness.


Declan Flynn Fitness
December 3, 2025 AT 06:31Been dealing with impetigo in my kid last winter - mupirocin worked like a charm. Just keep the area clean, no scratching, and don’t let them share towels. Simple stuff, but people overlook it. Also, moisturize dry skin like it’s your job. Eczema + heat = impetigo party.
Irving Steinberg
December 3, 2025 AT 22:04bro why are we still using antibiotics like it’s 2010 🤡 i’ve seen MRSA pop up in my gym locker room and no one even washes their hands anymore. just use tea tree oil and pray lol
Lydia Zhang
December 5, 2025 AT 19:20My niece got cellulitis after a mosquito bite. Took three days to get seen. She was in the hospital for a week. Don’t wait.
Michelle Smyth
December 6, 2025 AT 07:24How quaint - another post masquerading as clinical guidance while ignoring the structural determinants of skin infection disparities. The real issue isn’t antibiotic stewardship, it’s the commodification of primary care in neoliberal health systems. Mupirocin is a Band-Aid on a hemorrhage. Meanwhile, low-income families in rural Ireland and the American South are still scrubbing sores with dish soap because Medicaid won’t cover a dermatology consult. The microbiome is politicized. The skin is a frontier.
And yet, here we are, debating flucloxacillin vs. cephalexin as if resistance patterns were apolitical. The colonial legacy of antibiotic distribution persists. Who gets vancomycin? Who gets Neosporin? The answer is written in zip codes.
Let’s not pretend this is about science. It’s about access. And access is never neutral.
Also, tea tree oil has antimicrobial properties, but you’re not going to cure necrotizing fasciitis with lavender and intention. That’s just performative wellness.
And yes, I’ve read the 2023 Lancet study on antibiotic overuse. I also know that 70% of prescriptions are written without culture confirmation. That’s not stewardship. That’s triage capitalism.
But hey, at least we have tables now. So much data. So little justice.
Kay Lam
December 7, 2025 AT 01:25I work in a community clinic and I see this all the time. Parents come in thinking their kid’s impetigo is just a rash because it doesn’t hurt. They don’t realize how contagious it is. I always tell them to treat it like a virus - keep the child home, wash everything, don’t share combs or pillows. And if the crusts spread past the face? That’s not just impetigo anymore. That’s a red flag for deeper infection.
Cellulitis is even trickier. Elderly patients often think it’s just a bruise or a bug bite. I had one man come in with a swollen leg he’d been icing for three days. By the time he showed up, his WBC was through the roof. We had to start IV antibiotics right away. He’s lucky he didn’t lose the leg.
And no, OTC creams don’t cut it. I’ve seen people slather Neosporin on a honey-crusted sore for a week. It doesn’t help. It just makes it worse. Prescription mupirocin is the only thing that works for impetigo. And for cellulitis, you need something that covers strep and staph - not just a little tube from the drugstore.
Also, if you’re diabetic, check your feet every day. Like, every single day. Even if it’s just a tiny crack. That’s where cellulitis starts. I’ve lost count of how many amputations I’ve seen that could’ve been prevented with a 30-second check.
And please, stop sharing antibiotics. I had a woman bring in her husband’s leftover cephalexin for her son’s rash. It didn’t work. The kid ended up with MRSA. Now he’s on clindamycin. And we’re still trying to figure out how it got into the house.
Antibiotics aren’t candy. They’re precision tools. Use them right or don’t use them at all.
And yes, handwashing matters. It’s not just for hospitals. It’s for every home, every classroom, every gym. Wash your hands. It’s free. It’s simple. It saves lives.
Patrick Smyth
December 7, 2025 AT 20:40I remember when my daughter got impetigo - I was terrified. I thought it was poison ivy. I almost took her to the naturopath. Thank God I called the doctor. That honey crust? It looked like something out of a horror movie. I cried. I didn’t sleep. I washed every towel in the house three times. And now? I’m obsessed with hygiene. I carry hand sanitizer everywhere. I disinfect doorknobs. I don’t even let my kids touch each other’s faces anymore. I know it’s extreme. But I’d rather be paranoid than bury my child.
Matt Dean
December 8, 2025 AT 22:21People still don’t get it. Impetigo isn’t a ‘school sore’ - it’s a sign your kid’s environment is dirty. If your daycare doesn’t have a strict handwashing policy, get your kid out. Cellulitis? That’s your fault if you’re diabetic and never check your feet. Stop blaming the bacteria. Start blaming the negligence.
James Steele
December 9, 2025 AT 12:42Antibiotic resistance isn’t a medical problem - it’s a metaphysical crisis. We’ve turned the body into a battlefield of chemical warfare, and yet we refuse to acknowledge the existential toll. Mupirocin? A temporary truce. Vancomycin? A last gasp. The real question isn’t which drug to prescribe - it’s whether we’re willing to live in a world where infection is inevitable, and cure, merely a privilege.
And yet, we keep prescribing. Like monks chanting incantations over a dying altar.
Nnaemeka Kingsley
December 11, 2025 AT 11:16in nigeria we use local herbs sometimes but if it spread we go to clinic. my cousin had cellulitis after cut on leg - took 2 weeks to heal. doctor said dont wait. i think this post good. but maybe add more about africa? many people here dont have access to mupirocin. we use amoxicillin even for impetigo. its not ideal but its all we got.
Shashank Vira
December 12, 2025 AT 04:11One must question the epistemological foundations of antibiotic prescribing. The very notion of ‘first-line’ implies a hierarchy of truth that colonial medicine has imposed upon global health. Why is flucloxacillin the gold standard in the UK while pristinamycin reigns in France? Is it science - or hegemony? The microbiome does not recognize borders. Yet our protocols do. This is not medicine. It is cartography of control.
Tommy Walton
December 12, 2025 AT 07:38impetigo = staph party 🤡 cellulitis = staph gone full horror movie 🎬
Courtney Co
December 12, 2025 AT 19:04I had cellulitis after a pedicure. The salon didn’t sterilize the tools. I didn’t know it was dangerous. I just thought my foot was sore. Now I’m terrified of every little cut. I don’t even let my kids play outside without socks on. I’m not overreacting - I’m traumatized.
Adrian Barnes
December 12, 2025 AT 20:19The data presented is statistically sound, yet the underlying assumption - that clinical outcomes are primarily determined by antibiotic selection - is dangerously reductionist. One must account for socioeconomic determinants, microbial virulence dynamics, and the psychosocial impact of chronic skin pathology. The failure to contextualize these variables renders this article a mere symptom of biomedical hegemony. Furthermore, the omission of longitudinal recurrence rates and biofilm-mediated persistence mechanisms constitutes a critical scholarly lacuna. One would hope for peer-reviewed depth, not a public health pamphlet masquerading as medical authority.