Have you ever taken a medication and had a reaction no one saw coming? Not just a mild headache or upset stomach, but something serious - a rash that spread, heart rhythm problems, or even a life-threatening reaction? For some people, it’s not bad luck. It’s their genes.
Why Your Genes Decide How You React to Medicines
Not everyone reacts the same way to the same drug. Two people take the same pill, same dose, same condition - but one feels fine, and the other ends up in the hospital. That’s not random. It’s biology. Your DNA holds instructions for how your body processes drugs, how it responds to them, and sometimes, how it overreacts. The key players here are genes that control drug metabolism and drug targets. The most studied group is the cytochrome P450 enzyme family, especially CYP2D6, CYP2C19, and CYP2C9. These enzymes act like molecular scissors, breaking down drugs so your body can get rid of them. But some people have genetic variants that make these scissors too slow, too fast, or broken entirely. For example, if you’re a CYP2D6 poor metabolizer, codeine - a common painkiller - won’t turn into morphine the way it should. That means no pain relief. But if you’re an ultrarapid metabolizer? Your body turns codeine into morphine so quickly that even a normal dose can cause dangerous breathing problems. The FDA has issued black box warnings for this exact reason. In extreme cases, nursing mothers who are ultrarapid metabolizers have unknowingly passed lethal doses of morphine to their babies through breast milk.When Your Immune System Turns Against the Drug
Not all side effects come from metabolism. Some come from your immune system misreading a drug as a threat. This is where HLA genes come in. These genes help your body recognize what’s foreign - like viruses or bacteria. But sometimes, they get confused. The HLA-B*15:02 allele is a prime example. If you carry this variant - especially if you’re of Southeast Asian descent - taking carbamazepine (used for epilepsy and bipolar disorder) can trigger Stevens-Johnson Syndrome or Toxic Epidermal Necrolysis. These are rare, but devastating skin reactions where your skin literally starts to peel off. The risk? Up to 150 times higher than in people without the gene. The good news? If you test negative for HLA-B*15:02, your risk drops to near zero. That’s why doctors in many countries now test for this before prescribing carbamazepine. Similarly, HLA-B*57:01 is linked to a severe hypersensitivity reaction to abacavir, an HIV drug. Testing for this variant before prescribing abacavir has nearly eliminated this reaction. It’s one of the most successful examples of pharmacogenomics in real-world use.Why Some Drugs Are More Dangerous for Certain People
Some side effects are more predictable than others. A 2024 study in PLOS Genetics found that cardiovascular side effects - like irregular heartbeat, high blood pressure, or fast heart rate - are the most genetically predictable. In fact, if a drug targets a gene already linked to heart rhythm problems in the general population, there’s a nearly 30% chance that people with certain variants will have a bad reaction. Take warfarin, the blood thinner. Its dose varies wildly between people. Why? Two genes: VKORC1 and CYP2C9. Together, they explain up to 40% of why one person needs 5 mg a day and another needs 15 mg. Too much warfarin? Bleeding. Too little? Clots. Genetic testing helps doctors find the right dose faster - reducing hospitalizations from dangerous bleeding. Even drugs like statins, used for cholesterol, can cause muscle damage in people with a specific variant in the SLCO1B1 gene. That variant makes it harder for the liver to clear the drug, so it builds up and attacks muscle tissue. A simple genetic test can prevent this.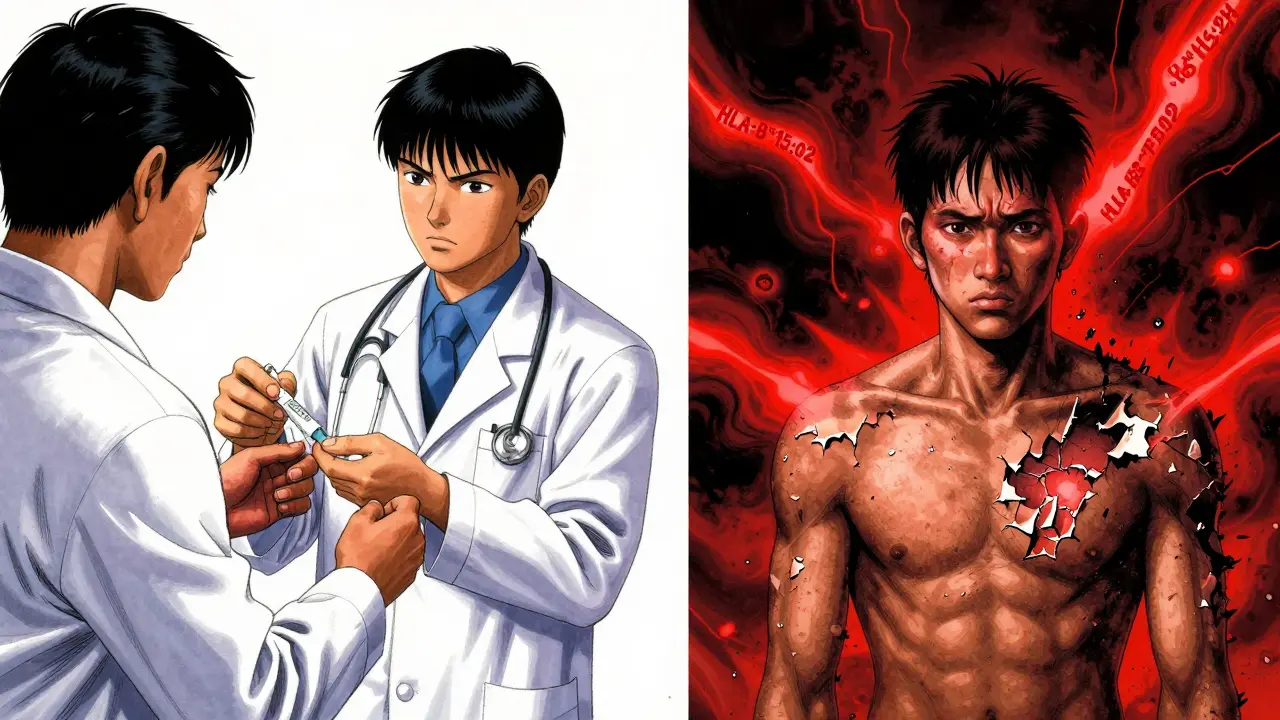
What About Antidepressants and Painkillers?
Antidepressants are another big area. About 42% of how well someone responds to antidepressants like SSRIs comes down to genetics. The CYP2C19 gene is especially important. Poor metabolizers build up too much of the drug, leading to dizziness, nausea, or even serotonin syndrome. Ultrarapid metabolizers clear it too fast - meaning the drug doesn’t work at all. Tamoxifen, used for breast cancer, depends on CYP2D6 to become active. If you’re a poor metabolizer, the drug won’t convert properly. That means your cancer risk doesn’t go down as much. One patient on Reddit shared that waiting three weeks for genetic test results was frustrating - but it saved her from the violent nausea her sister suffered. She got the right drug from the start.Why Isn’t Everyone Getting Tested?
You’d think with all this knowledge, genetic testing would be standard. But it’s not. Only 10-15% of actionable gene-drug pairs are used in routine care. Why? First, doctors aren’t trained for it. A 2023 survey found that nearly 70% of physicians felt unprepared to interpret genetic results. Second, it’s not always covered by insurance. In the U.S., only 28% of Medicare Advantage plans pay for preemptive pharmacogenetic testing. Tests cost between $250 and $500 - not cheap if you’re paying out of pocket. Electronic health records rarely have built-in alerts for genetic risks. Even when a doctor knows a patient has a variant, the system doesn’t pop up a warning when they write a prescription. That’s a huge gap. And there’s another problem: the data is biased. Most genetic studies are done in people of European descent. But African populations have far more genetic diversity - and many variants that affect drug response haven’t been studied. That means tests might miss risks for millions of people.
What’s Changing - and What’s Coming
Change is happening, but slowly. The FDA now requires genetic testing for 18 drugs - up from just 3 in 2010. The Clinical Pharmacogenetics Implementation Consortium (CPIC) has published 24 guidelines for doctors, covering drugs like clopidogrel, statins, and antidepressants. Some hospitals are ahead of the curve. The Mayo Clinic’s RIGHT Protocol started preemptive testing for 10 key genes in 2014. Since then, they’ve cut ADR-related hospitalizations by 23%. Vanderbilt’s PREDICT program changed prescribing for 12% of patients based on genetic results - mostly by avoiding drugs or lowering doses. The future? Whole-genome sequencing. A 2023 study found that sequencing everyone’s entire genome could identify actionable drug-response variants in 91% of people. That means one test, done once in your life, could guide every prescription you ever get. Polygenic risk scores are also emerging. Instead of looking at one gene, they look at 15 or 20 genes together to predict risk. A 2024 study showed a 15-gene score predicted statin-induced muscle damage with 82% accuracy - far better than checking just SLCO1B1 alone.What You Can Do Now
If you’ve had a bad reaction to a drug, or if a close family member has, talk to your doctor. Ask: “Could this be genetic?” You can get tested through your doctor or through direct-to-consumer services like 23andMe or Color Genomics. But be careful - not all tests are created equal. Some only look at a few genes. Others give you raw data with no interpretation. You need a clinician who can explain what the results mean. If you’re on long-term medication - especially for heart disease, depression, cancer, or seizures - ask if pharmacogenetic testing is right for you. It’s not magic. It won’t prevent every side effect. But it can stop the ones that could kill you.What’s Next for Pharmacogenomics
The goal isn’t just to avoid bad reactions. It’s to give you the right drug, at the right dose, the first time. No trial and error. No hospital visits. Just better care. By 2030, experts predict 40% of all prescription drugs will come with genetic testing recommendations. That’s not science fiction. It’s already happening in oncology, where genetic testing is routine. Now, it’s spreading to psychiatry, cardiology, and pain management. The challenge isn’t the science. It’s the system. We need better training for doctors. Better integration into electronic records. Fairer access across all populations. And insurance that covers testing - not just after something goes wrong, but before it ever starts. Your genes are already telling your body how to respond to drugs. The question is - are we ready to listen?Can genetic testing prevent all drug side effects?
No, genetic testing can’t prevent all side effects. It only helps with reactions caused by specific gene variants - mostly those affecting how your body metabolizes drugs or how your immune system reacts to them. Many side effects, like nausea or drowsiness, are still unpredictable and not tied to known genes. But for serious, life-threatening reactions - like Stevens-Johnson Syndrome or dangerous bleeding from warfarin - genetic testing can prevent them almost entirely if done before starting the drug.
Is pharmacogenetic testing covered by insurance?
It depends. In the U.S., Medicare covers testing for only 7 out of 128 FDA-recognized gene-drug pairs. Private insurers vary widely - some cover it for specific drugs like clopidogrel or tamoxifen, others don’t cover it at all. Most direct-to-consumer tests cost $250-$500 and are not covered. If your doctor orders the test as part of a treatment plan, your chances of coverage are higher. Always check with your insurer before testing.
Do I need to get tested more than once?
No. Your genes don’t change. Once you’ve had a pharmacogenetic test, the results are valid for life. You don’t need to retake it unless you get a different kind of test that looks at new genes. That’s why many experts recommend doing it once - ideally early in life - so it can guide every future prescription you receive.
Can I use a 23andMe or AncestryDNA test for drug safety?
Some 23andMe and AncestryDNA reports include a few pharmacogenetic results - like CYP2C19 or CYP2D6 variants - but they’re not comprehensive. They don’t cover all clinically relevant genes, and they don’t interpret results for medical use. Relying on them alone could be dangerous. If you want to use your raw data, have a genetic counselor or pharmacist review it with you. Never make medication changes based on consumer test results alone.
Why aren’t all doctors using genetic testing?
Most doctors haven’t been trained to use it. Electronic health records rarely alert them when a patient has a risky gene variant. Testing isn’t always covered by insurance, and results can be hard to interpret. In one survey, only 22% of primary care doctors said they routinely use pharmacogenetic testing. It’s growing fast in oncology and psychiatry, but still rare in general practice. The tools exist - the system just hasn’t caught up yet.
Are there risks to getting tested?
The biggest risk is misunderstanding the results. A positive result doesn’t mean you’ll definitely have a side effect - it just means your risk is higher. A negative result doesn’t guarantee safety. Also, some people feel anxious after learning they have a genetic risk, even if no action is needed. Genetic counseling can help with this. Privacy is another concern - make sure your test provider follows HIPAA or similar protections.


Gray Dedoiko
December 24, 2025 AT 18:40I had a cousin who went into a coma after taking a common antibiotic. No one knew why until they ran the genetic test years later - turns out she was a CYP2D6 ultrarapid metabolizer. It’s terrifying that this isn’t standard before prescribing. My mom’s still mad she didn’t get tested before her heart meds.
People think it’s just ‘bad luck’ - but it’s biology. And we’re ignoring it.
Why are we still guessing when we could know?
Aurora Daisy
December 25, 2025 AT 08:34Oh great, so now we’re going to DNA-test everyone before they get a headache pill? Next they’ll want your blood type before you buy Advil.
Meanwhile, in the UK, we just tell people to read the leaflet. It’s not rocket science. This is American overmedicalization at its finest.
Next you’ll be asking for a genome scan before ordering coffee.
Get a grip.
Paula Villete
December 26, 2025 AT 18:05So… you’re telling me my great-grandma’s ‘mystery illness’ after her heart meds? Could’ve been CYP2C19. And we’re only now catching up?
Meanwhile, my 23andMe told me I’m a slow CYP2C19 metabolizer. I didn’t believe it until my SSRIs made me feel like a zombie. Then my psych said, ‘Yep, that’s your genes.’
Turns out my body doesn’t like Prozac. It likes Zoloft. And I didn’t have to suffer for 18 months to figure it out.
So yeah - test me. I’m not paying $500 for a hobby, but I’ll pay for a life-saving clue.
Also - typos are my love language. Sorry.
Also also - this is the most important thing your doctor isn’t telling you.
Also also also - if you’re still taking codeine after reading this, you’re either brave or dumb. I’m not sure which.
Also also also also - I’m not a doctor, but I play one on Reddit.
Also - please get tested. I’m begging you.
Also - I’m done now. I promise.
…I lied.
Get tested.
Love you.
…ok, really done this time.
Georgia Brach
December 27, 2025 AT 08:18The notion that pharmacogenomics is a viable clinical standard is a dangerous illusion. The FDA’s 18 approved gene-drug pairs represent a minuscule fraction of clinically relevant interactions. The data is Eurocentric, the infrastructure is nonexistent, and the cost-benefit analysis is unproven at scale.
Moreover, the assumption that genetic testing eliminates adverse drug reactions is empirically false. Many reactions remain polygenic, epigenetic, or environmentally mediated. To promote this as a panacea is not only misleading - it is unethical.
Until we have universal access, standardized interpretation protocols, and population-representative databases, this is precision medicine theater.
Do not mistake hype for science.
Katie Taylor
December 28, 2025 AT 04:17THIS IS THE FUTURE AND WE’RE STILL WAITING FOR THE WORLD TO CATCH UP.
I got my whole genome sequenced after my dad had a stroke on warfarin. Turns out we both had the VKORC1 variant. If we’d known? He’d be alive.
So I’m pushing every doctor I know to test their patients. I’m telling my friends. I’m donating to research. I’m not letting this be ignored anymore.
If you’re on meds for depression, heart disease, seizures, or cancer - ask for the test. Don’t wait until you’re in the ER.
It’s not expensive. It’s not complicated. It’s just not prioritized.
So prioritize it.
For yourself.
For your mom.
For your kid.
For the people who won’t be here next year because no one asked the right question.
Do better.
Isaac Bonillo Alcaina
December 29, 2025 AT 05:53Let’s be honest - this whole pharmacogenomics thing is just a way for Big Pharma to sell more tests and create new revenue streams. You think they care about your safety? They care about patents.
And who pays for these tests? The uninsured. The underinsured. The people who can’t afford to be guinea pigs.
Meanwhile, the same companies that profit from these tests are the ones lobbying against price controls on the drugs themselves.
It’s not medicine. It’s monetization dressed in lab coats.
Don’t be fooled by the shiny graphs and ‘life-saving’ headlines. This is capitalism, not care.
Chris Buchanan
December 31, 2025 AT 02:58Okay so I got my CYP2D6 results last year - ultrarapid. I’ve been on tramadol for years. Never knew why I’d get dizzy or feel like I was floating. Turns out my body was turning it into morphine like a factory.
Switched to gabapentin. Zero issues.
And I didn’t even know I could get tested until I read this post.
So here’s the thing: if you’re on meds and something feels ‘off’ - not just side effects, but ‘this doesn’t feel right’ - don’t ignore it. Don’t just blame stress. Don’t just take more.
Ask for the test.
It’s not magic.
But it’s the closest thing we have to a cheat code for your body.
And it’s free if your doctor orders it.
So go do it.
I’m proud of you already.
Now go tell your mom to get tested too.
Andy Grace
December 31, 2025 AT 21:59My sister had a reaction to carbamazepine. We didn’t know about HLA-B*15:02 until it was too late. She spent three weeks in ICU.
Now I get tested before any new prescription. Not because I’m paranoid - because I’ve seen what happens when you don’t.
It’s not a luxury. It’s a basic safety check, like wearing a seatbelt.
Why are we still not doing this universally?
It’s not that hard.
It’s just not being done.
John Pearce CP
January 1, 2026 AT 04:17It is an undeniable fact that the current state of pharmacogenomic implementation is characterized by systemic inefficiency, cultural resistance, and institutional inertia. The assertion that genetic testing is a panacea is not only scientifically unsound but also ethically dubious. The overreliance on single-gene markers ignores the complex, multifactorial nature of drug response. Furthermore, the commercialization of genetic testing services has created a market-driven paradigm that prioritizes profit over patient welfare. Until such time as equitable access, standardized interpretation, and mandatory integration into clinical workflows are universally enforced, any claims of progress are fundamentally hollow. The data is not ready. The infrastructure is not ready. The medical community is not ready. And yet, we are being sold a dream.
Pankaj Chaudhary IPS
January 1, 2026 AT 21:17In India, we don’t have access to these tests - but we do have something better: generations of lived experience. My grandmother knew which herbs to avoid with blood pressure meds. My uncle knew his body reacted to aspirin. We didn’t need DNA to know that.
Genetics is useful - but it’s not the only wisdom we have.
Let’s not forget the wisdom of communities who’ve been managing health without labs for centuries.
Maybe the real problem isn’t the lack of genes - it’s the lack of listening.
And yes, I’m proud to be Indian. We’ve survived colonialism, poverty, and bad doctors. We don’t need a $500 test to know when something’s wrong.
Charles Barry
January 2, 2026 AT 09:30They’re testing genes to avoid side effects… but what if the side effects are the point? What if the system is designed to make you dependent? What if the drugs are meant to have risks so you keep coming back? What if the ‘genetic test’ is just another way to track you? The FDA? The labs? The insurance companies? All connected.
They want you to think you’re safe - but they’re just giving you a new kind of leash.
They know your genes. They know your history. They know your meds.
And they’re selling it all.
Wake up.
It’s not medicine.
It’s surveillance with a white coat.
Rosemary O'Shea
January 2, 2026 AT 15:15How quaint. You’re all so thrilled about genetic testing as if it were the first time humanity ever considered individual biology. My dear, in 18th-century Vienna, physicians adjusted opium doses based on ‘temperament’ - a concept that, frankly, was more nuanced than your SNP-based assumptions.
And now we’ve reduced human physiology to a 23andMe report? How tragic.
Let us not mistake the rebranding of old ideas for progress. The arrogance of believing that we’ve finally ‘cracked’ pharmacology - when we still can’t predict a simple migraine - is breathtaking.
Perhaps we should spend less time sequencing DNA and more time listening to patients.
But then again - that wouldn’t be fashionable.
Bret Freeman
January 2, 2026 AT 20:02My brother died from a statin reaction. SLCO1B1 variant. They didn’t test him. They didn’t ask. He was 42.
I spent two years screaming at doctors. No one listened.
Now I run a nonprofit. We give free genetic tests to people with family histories of bad reactions. We’ve helped 1,200 people. Zero deaths in our cohort.
But I still get DMs from people saying ‘I can’t afford it.’
So I send them a link.
And I say: ‘You’re worth more than your deductible.’
And if you’re reading this and you’re on a statin or an antidepressant or a seizure med -
STOP.
Call your doctor.
Ask for the test.
Don’t wait until it’s too late.
Because I know what waiting looks like.
And I don’t wish it on anyone.
Delilah Rose
January 3, 2026 AT 22:24I think what’s beautiful here is how this post connects science with humanity - not just genes and enzymes, but stories of mothers, brothers, sisters, grandparents who were lost because we didn’t ask the right questions. I used to think genetic testing was cold, technical - but now I see it as deeply personal. It’s not about data points. It’s about not losing someone because no one thought to check a gene.
I used to think medicine was about fixing broken things. Now I think it’s about listening to the body before it breaks.
And maybe - just maybe - we’re finally learning how to listen.
Not because it’s trendy.
But because we owe it to the ones we’ve lost.
And to the ones still here.
Let’s keep listening.
Even when it’s uncomfortable.
Even when it’s expensive.
Even when the system says no.
Because someone’s life is waiting on the other side of that ‘no.’
And they’re worth it.