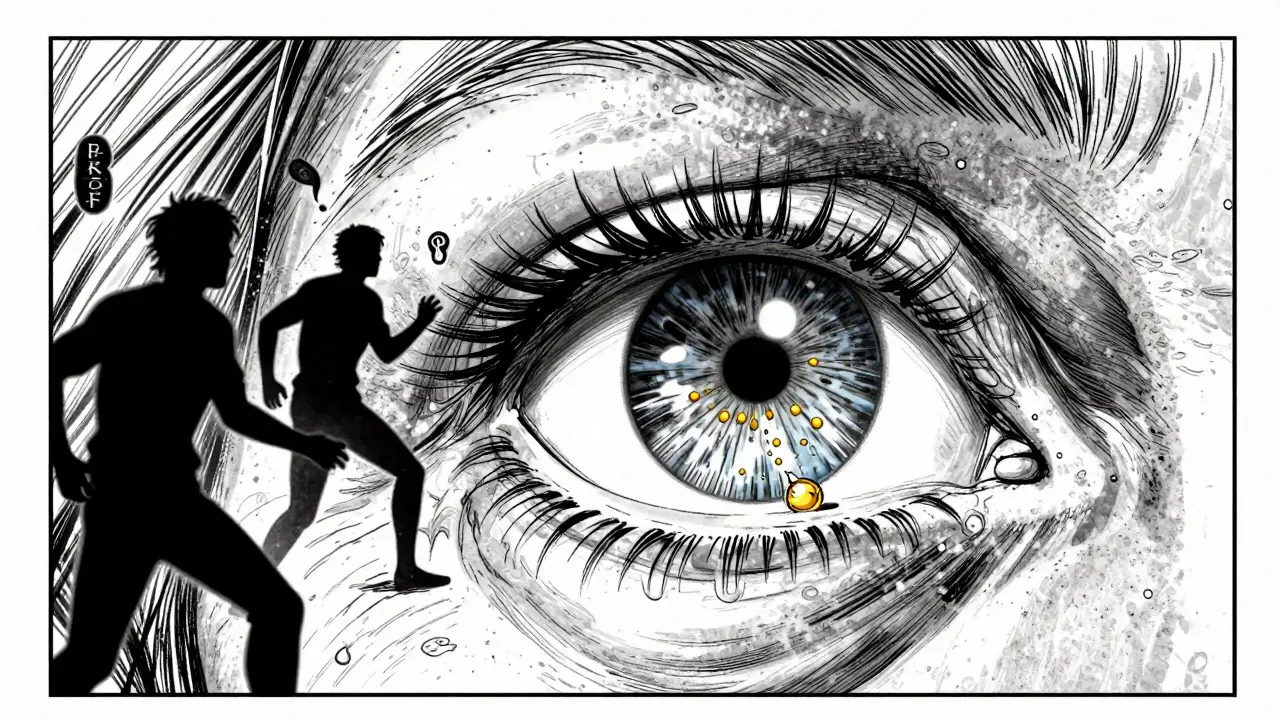
What Is Retinal Vein Occlusion?
Retinal vein occlusion (RVO) happens when a vein in the retina gets blocked, stopping blood from flowing out. This causes fluid to leak into the retina, leading to swelling - especially in the macula, the part of the eye responsible for sharp central vision. The result? Sudden, painless blurring or loss of vision in one eye. It doesn’t happen overnight for most people; it’s the end result of years of underlying health issues.
There are two main types: central retinal vein occlusion (CRVO), which blocks the main vein, and branch retinal vein occlusion (BRVO), which affects smaller branches. BRVO is more common and often occurs where a hardened artery crosses over a vein, pinching it shut. CRVO tends to be more severe and carries a higher risk of permanent vision loss.
Who’s Most at Risk?
Age is the biggest factor. Over 90% of CRVO cases happen in people over 55, and more than half of all RVO cases occur in those over 65. But it’s not just an older person’s disease - about 5 to 10% of cases strike people under 45, often with different triggers.
Here’s what actually increases your risk:
- Hypertension: Present in up to 73% of CRVO patients over 50. Uncontrolled high blood pressure is the #1 driver of vein blockages in the eye.
- Diabetes: Affects about 10% of RVO patients over 50. It damages small blood vessels over time, making them more prone to clots.
- High cholesterol: Total cholesterol above 6.5 mmol/L is found in 35% of RVO patients, regardless of age. It contributes to artery hardening, which squeezes retinal veins.
- Glaucoma: High pressure inside the eye, especially when it’s elevated near the optic nerve, increases the chance of vein compression.
- Smoking: Found in 25-30% of cases. It thickens blood and damages blood vessel walls.
- Obesity and inactivity: These promote inflammation and poor circulation, both of which worsen vascular health.
For women under 45, oral contraceptives are a known trigger - especially for CRVO. Blood disorders like polycythemia vera, multiple myeloma, or inherited clotting conditions (like factor V Leiden) also raise risk in younger patients.
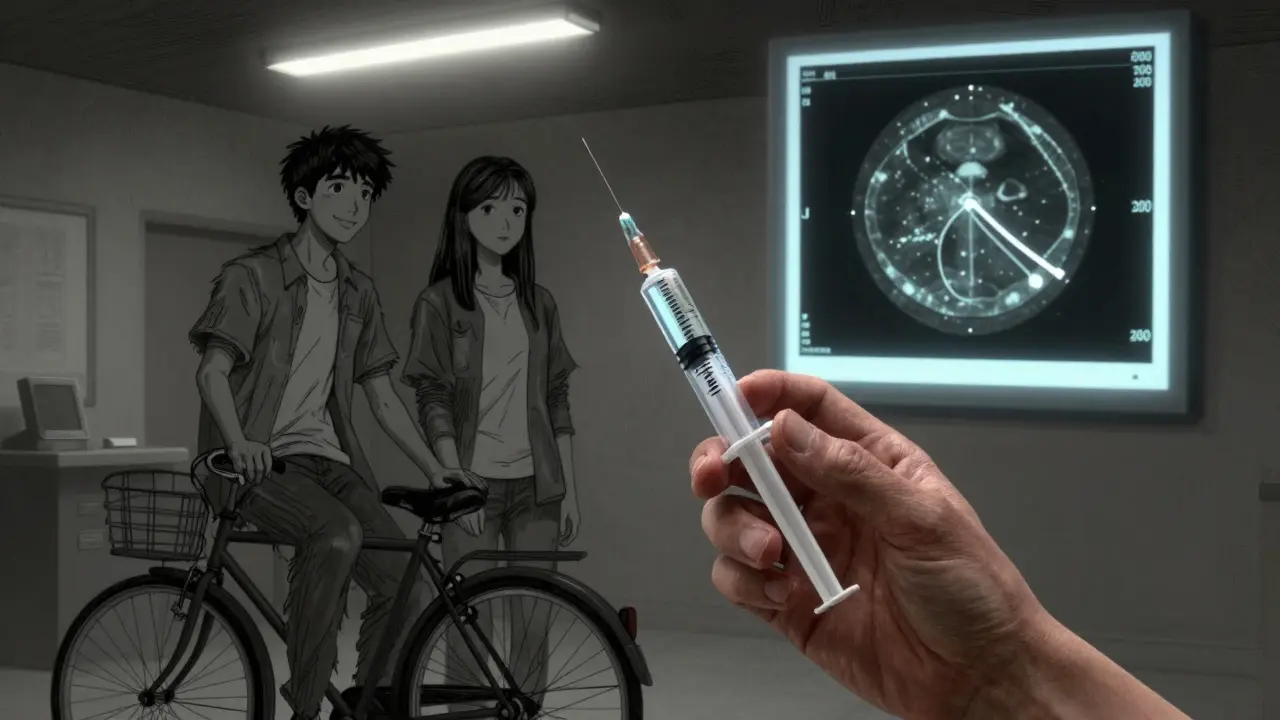
How Is It Diagnosed?
If you suddenly notice blurred vision in one eye, don’t wait. An eye doctor will do a few key tests:
- Visual acuity test: Measures how well you see at different distances.
- Fundoscopy: The doctor looks directly at the back of your eye using a special magnifier. Swollen, dilated veins and bleeding are clear signs.
- Optical coherence tomography (OCT): This non-invasive scan shows fluid buildup in the retina. It’s the gold standard for tracking macular edema - treatment decisions are based on whether the central retinal thickness exceeds 300 micrometers.
- Fluorescein angiography: A dye is injected into your arm, and photos are taken as it flows through the eye’s blood vessels. This reveals exactly where the blockage is and how much leakage is happening.
OCT is especially important because it’s used to guide treatment. Doctors don’t just treat based on how blurry your vision is - they look at the actual fluid levels in your retina.
What Are the Main Treatments?
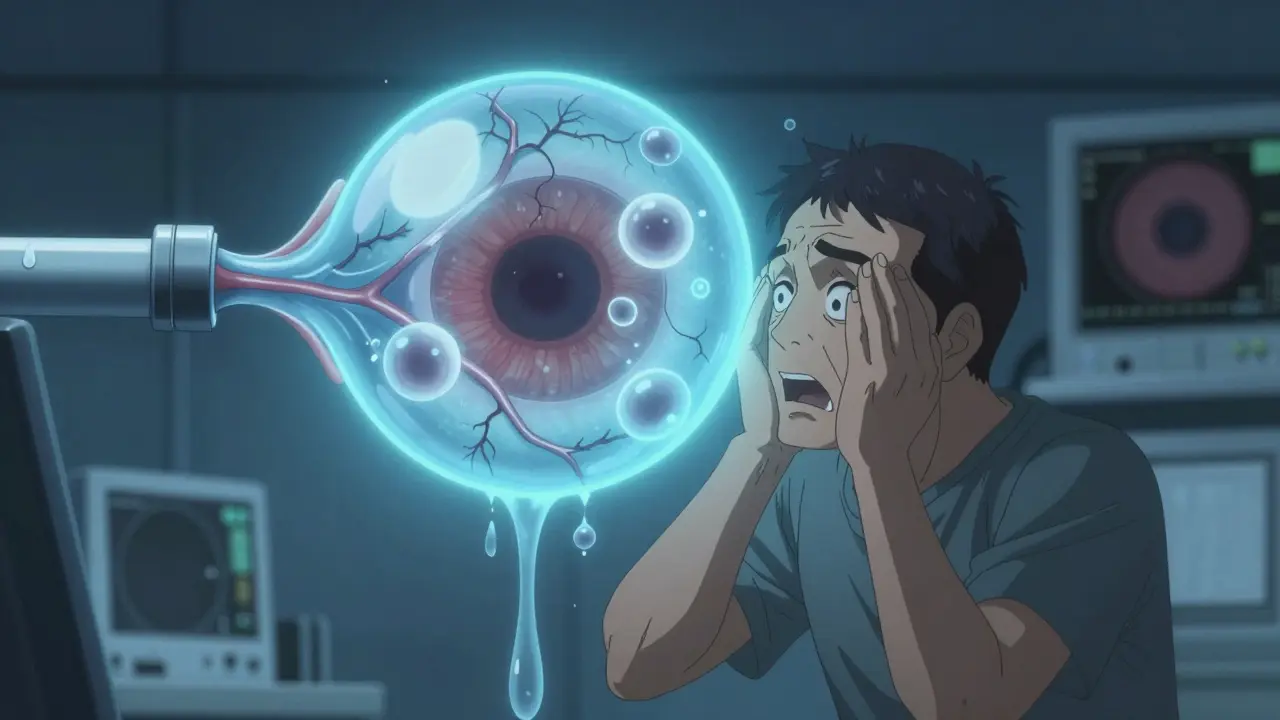
There’s no way to unblock the vein. Treatment focuses on reducing swelling and preventing further damage. The two main tools are injections directly into the eye.
Anti-VEGF Injections
These are the first-line treatment for most patients. They block a protein called VEGF that causes blood vessels to leak fluid. Three drugs are used:
- Ranibizumab (Lucentis): Approved specifically for RVO. Clinical trials showed patients gained an average of 16.6 letters on the eye chart after 12 months.
- Aflibercept (Eylea): Also FDA-approved. In trials, patients improved by 18.3 letters on average at six months.
- Bevacizumab (Avastin): Originally developed for cancer, it’s used off-label for RVO. It costs about $50 per dose versus $2,000 for the others. Many safety-net clinics use it because it’s effective and affordable.
Typical treatment starts with monthly injections until the fluid in the retina drops below 250 micrometers. After that, you switch to an as-needed schedule. Real-world data shows most patients need 8 to 12 injections per year to maintain vision.
Corticosteroid Injections
For patients who don’t respond well to anti-VEGF, or who have more inflammation, doctors may use steroid implants like Ozurdex. This is a tiny, biodegradable pellet injected into the eye that slowly releases dexamethasone over 3-6 months.
The GENEVA trial showed 27.7% of CRVO patients gained 15 or more letters of vision with Ozurdex, compared to 12.9% with placebo. But there’s a trade-off: up to 70% of patients develop cataracts, and 30% get elevated eye pressure that needs medication.
What Do Patients Really Experience?
Real life doesn’t always match clinical trial results.
One patient, 62, started monthly Lucentis injections after CRVO. By month four, his vision improved from 20/200 to 20/60 - a huge win. But the $150 copay per shot added up fast on a fixed income.
Another patient tried eight Avastin injections with little progress. Then she got the Ozurdex implant. Within weeks, her vision jumped 10 lines. She paid $2,500 out of pocket, but said it was worth it.
But the emotional toll is real. Many patients describe anxiety before each injection - even though the procedure takes less than 10 minutes. One Reddit user wrote: "My heart races every time, even though I know it’s routine. I’ve had 20 of them. I still hate it."
Some people stop coming. After 18 months of monthly shots, one patient developed such severe injection anxiety she started missing appointments - even though her vision kept improving. Treatment fatigue is a major reason people fall out of care.
What’s New in RVO Treatment?
The field is moving fast. A 2023 study called COMINO showed that a "treat-and-extend" approach - starting with monthly shots, then slowly extending the time between them if the eye stays stable - works just as well as monthly dosing but cuts injection frequency by 30%.
Another breakthrough: OPT-302, a new drug that blocks two forms of VEGF (C and D), is being tested in combination with aflibercept. Early results suggest it helps patients who didn’t respond to anti-VEGF alone.
Gene therapy is on the horizon. RGX-314, a one-time injection that makes the eye produce its own anti-VEGF protein, is in Phase II trials. If it works, patients could avoid injections entirely after one treatment.
And then there’s the Port Delivery System (Susvimo), a tiny implant that slowly releases ranibizumab over months. Approved for AMD, it’s now being tested for RVO. If approved, it could mean quarterly instead of monthly visits.
What Should You Do After Diagnosis?
Getting an RVO diagnosis isn’t the end - it’s a wake-up call. Your eye doctor will treat the swelling, but you need to fix what caused it.
Here’s what to do next:
- Control your blood pressure. Aim for under 130/80. This is the single most important step.
- Manage your blood sugar. If you have diabetes, HbA1c should be below 7%.
- Lower your cholesterol. Statins aren’t just for heart health - they help your retinal vessels too.
- Quit smoking. Every cigarette you don’t smoke reduces your risk of recurrence.
- Get regular eye checkups. Even if your vision feels fine, fluid can build up silently. OCT scans every 3-6 months are essential.
And don’t ignore the emotional side. Talk to your doctor about injection anxiety. Some clinics offer counseling or support groups. You’re not alone.
What’s the Long-Term Outlook?
With treatment, 30-40% of patients regain vision to 20/40 or better - enough to drive and read normally. But without treatment, many lose vision permanently.
Recurrence is possible. About 10-15% of patients have another RVO in the same or opposite eye within five years. That’s why managing your overall vascular health matters more than the injection schedule.
The future is personalized. Doctors are starting to use OCT angiography to look at blood flow patterns in the retina. That will help predict who responds to which drug - and who might need a combination approach.
Can retinal vein occlusion be cured?
No, RVO can’t be cured - the blocked vein doesn’t reopen. But treatment can stop further damage and restore lost vision in many cases. The goal is to manage the complications, especially macular edema, and prevent recurrence by controlling underlying health conditions.
Are eye injections painful?
Most patients feel only mild pressure or a brief sting. The eye is numbed with drops, and the needle is very thin. The whole process takes under 10 minutes. The anxiety before the injection is usually worse than the procedure itself.
How many injections will I need?
It varies. Most patients start with monthly injections for 3-6 months, then switch to as-needed dosing. On average, people need 8-12 injections per year. New protocols like treat-and-extend can reduce that number by 30% without losing results.
Can I use bevacizumab (Avastin) instead of Lucentis or Eylea?
Yes, and many doctors do. Avastin is used off-label for RVO and has similar effectiveness in clinical studies. It costs about 40 times less than the branded drugs. However, not all insurance plans cover it for eye use, and some clinics avoid it due to regulatory concerns - even though it’s widely used and safe.
What happens if I miss an injection?
Missing doses can lead to fluid building up again, causing vision to worsen. If you miss one, call your doctor right away. Don’t wait until your next scheduled visit. In many cases, you can resume treatment without long-term damage - but the longer you wait, the harder it is to recover lost vision.
Can retinal vein occlusion affect both eyes?
Yes, though it usually starts in one eye. About 10-15% of patients develop RVO in the other eye within five years. That’s why controlling risk factors like high blood pressure and cholesterol is so important - it protects both eyes.
Next Steps: Managing RVO for Life
Think of RVO like high blood pressure for your eyes. You can’t fix the blocked vein, but you can stop it from happening again. That means regular checkups, strict control of your blood pressure, cholesterol, and blood sugar, and sticking with your injection schedule - even when your vision feels fine.
The good news? Most people who stay on track maintain useful vision for decades. The bad news? Skipping care leads to irreversible damage. This isn’t a one-time fix. It’s a lifelong commitment - but one that lets you keep reading, driving, and seeing the people you love.

Jennifer Phelps
January 12, 2026 AT 02:29jordan shiyangeni
January 13, 2026 AT 08:26Abner San Diego
January 15, 2026 AT 04:19Eileen Reilly
January 16, 2026 AT 12:21steve ker
January 16, 2026 AT 23:30Sonal Guha
January 18, 2026 AT 22:01TiM Vince
January 19, 2026 AT 03:41Alice Elanora Shepherd
January 19, 2026 AT 17:39Christina Widodo
January 20, 2026 AT 04:51Prachi Chauhan
January 20, 2026 AT 06:12Sona Chandra
January 21, 2026 AT 22:38Rinky Tandon
January 22, 2026 AT 13:45Ben Kono
January 22, 2026 AT 14:09