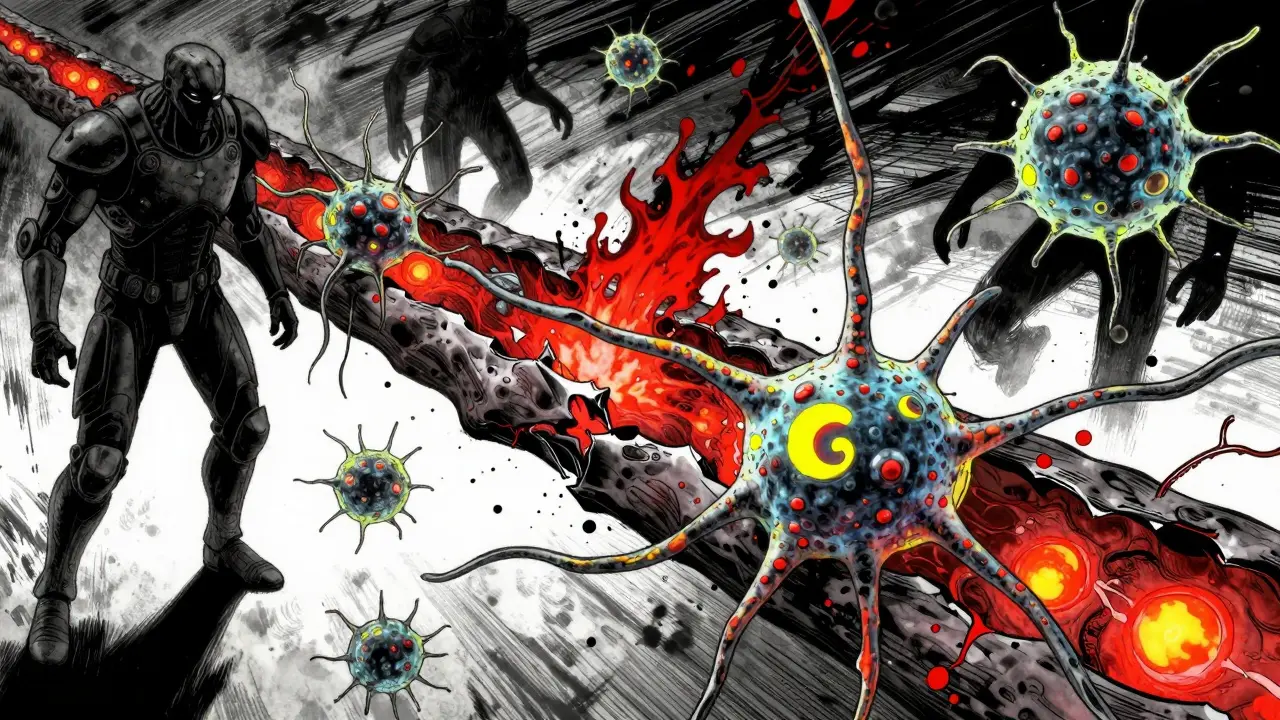
Multiple sclerosis isn’t just a neurological condition-it’s an inside job. Your own immune system, designed to protect you, turns against your brain and spinal cord. It sees the protective coating around your nerves as a threat and starts tearing it apart. That coating? Myelin. And when it’s gone, signals between your brain and body get scrambled. That’s when numbness, vision loss, fatigue, or trouble walking shows up-not because of injury, but because your body attacked itself.
What Happens When the Immune System Goes Rogue
In multiple sclerosis, the immune system launches a targeted assault on the central nervous system. The main target? Myelin, the fatty sheath that wraps around nerve fibers like insulation on an electrical wire. Without it, nerve signals slow down or stop entirely. This isn’t random damage. It’s precise. Immune cells-mainly T cells and B cells-cross the blood-brain barrier, a normally tight seal that keeps harmful substances out of the brain. Once inside, they recognize myelin as foreign and begin attacking. Research shows that in people with MS, these immune cells don’t just wander in. They’re activated elsewhere in the body, often triggered by environmental factors like the Epstein-Barr virus. Once they enter the CNS, they recruit more immune troops: macrophages, microglia, and dendritic cells. These cells release inflammatory chemicals that turn the area into a war zone. The result? Inflammation, swelling, and the destruction of myelin. Over time, the nerves themselves start to fray and die.The Four Patterns of Damage
Not all MS is the same. Scientists have identified four distinct patterns of tissue damage in the brain and spinal cord. Pattern I is mostly T cells and macrophages chewing through myelin. Pattern II adds antibodies to the mix-like the immune system is using a missile instead of a knife. Pattern III shows a different story: oligodendrocytes, the cells that make myelin, are dying off first. And Pattern IV? That’s the most alarming. Oligodendrocytes are damaged, but there’s no sign of immune cells nearby. It suggests something deeper is broken in the brain’s ability to repair itself. These patterns help explain why some people respond to certain treatments and others don’t. If your MS looks like Pattern II, drugs that target antibodies might help. If it’s Pattern III, the focus needs to shift to protecting or replacing myelin-making cells. This is why one-size-fits-all treatments often fail.Why Women Are More Affected
Women are two to three times more likely to develop MS than men. That gap is wider in places like Canada and Scandinavia, where rates can hit 140 cases per 100,000 people. Why? It’s not just hormones. While estrogen and progesterone play a role in immune regulation, the bigger story involves genetics and environment. Women’s immune systems tend to be more reactive-a trait that helped our ancestors survive infections during pregnancy. But that same sensitivity makes them more vulnerable to autoimmune misfires. Add in vitamin D deficiency (common in northern latitudes), smoking, and Epstein-Barr virus exposure, and you’ve got a perfect storm. People who carry certain genes like HLA-DRB1*15:01 and get infected with EBV before age 20 have a 32-fold higher risk of developing MS. It’s not one thing. It’s a chain reaction.
What You Feel When the Nerves Are Under Attack
Symptoms aren’t random. They map directly to where the damage happens. If the optic nerve is hit, you get optic neuritis-vision blurs, colors fade, pain shoots behind the eye. That’s not an eye problem. That’s an immune attack on the nerve connecting your eye to your brain. Fatigue? It affects 80% of people with MS. It’s not just tiredness. It’s like your body’s battery is draining even when you’re sleeping. That’s because your nerves are working overtime to send signals without myelin. Every movement, every thought, costs more energy. Numbness or tingling? That’s demyelination in the spinal cord. Walking becomes harder because your brain can’t tell your legs where to move. Lhermitte’s sign-the electric shock feeling when you bend your neck-is a classic sign. It means your cervical spine is damaged. When you move, the exposed nerve fires off a jolt of electricity. And it’s not just physical. Brain fog, depression, and trouble concentrating are common. The immune system isn’t just attacking nerves-it’s changing how the brain functions.How Treatments Fight Back
Today’s MS treatments don’t cure the disease. But they stop the immune system from doing so much damage. Disease-modifying therapies (DMTs) are the backbone of care. Ocrelizumab, for example, targets CD20+ B cells. In clinical trials, it cut relapses by 46% and slowed disability progression by 24% in primary progressive MS. Natalizumab blocks immune cells from crossing the blood-brain barrier. It reduces relapses by 68%, but carries a rare but serious risk: progressive multifocal leukoencephalopathy (PML), a brain infection caused by a dormant virus reactivating. Newer drugs like siponimod and cladribine work differently. They trap immune cells in lymph nodes or wipe out overactive ones. Each drug has trade-offs. Some require regular infusions. Others are pills with strict monitoring. The goal isn’t just to reduce flares-it’s to prevent long-term disability.
The Hope for Repair
The biggest breakthroughs might come from repair, not just suppression. For decades, scientists thought the brain couldn’t fix itself after myelin damage. Now we know it can-but only if the environment allows it. In relapsing-remitting MS, the brain tries to remyelinate. But the inflammation is too toxic. Oligodendrocyte precursor cells sit idle, waiting for the right signal. Clemastine fumarate, a common antihistamine, showed promise in a phase II trial. It improved nerve signal speed by 35% in people with MS. That’s not a cure. But it’s proof the brain can heal-if we give it the right conditions. Researchers are now testing drugs that block specific inflammatory signals like IL-21 and TNF-α. Others are exploring stem cell therapies to rebuild myelin. And biomarkers like serum neurofilament light chain (sNfL) are helping doctors see inflammation before symptoms appear. If sNfL levels rise above 15 pg/mL, it means active damage is happening-even if the patient feels fine.What’s Next
The future of MS care is personal. No two people have the same immune profile. Soon, doctors may test your blood for specific immune cell signatures, viral exposure history, and genetic markers to choose your treatment before you even have a relapse. The International Progressive MS Alliance has poured $65 million into research since 2014. Projects are underway in 14 countries, studying how dendritic cells present myelin to T cells, how neutrophil traps break down the blood-brain barrier, and why some people progress while others stay stable. The message is clear: MS isn’t just a disease of the nervous system. It’s a disease of immune miscommunication. And the best way to stop it isn’t to suppress the whole system-it’s to teach it what not to attack.Living With MS Today
People with MS are living longer, healthier lives than ever before. In the past, half of untreated RRMS patients needed a cane or walker within 15 to 20 years. Today, with early treatment, that number has dropped to about 30%. Many stay active, work full-time, raise families. It’s not easy. But the tools are better. The science is faster. And the understanding of what’s really happening inside the body has never been clearer. It’s still a battle. But now, the body’s own defenses aren’t always the enemy. Sometimes, they’re the key to healing-if we know how to listen.Is multiple sclerosis hereditary?
MS isn’t directly inherited like a genetic disorder, but having a close relative with MS increases your risk. If a parent or sibling has it, your chance rises to about 2-5%, compared to 0.1% in the general population. Specific genes like HLA-DRB1*15:01 play a role, but they only raise risk if combined with environmental triggers like Epstein-Barr virus or low vitamin D. No single gene causes MS-it’s a mix of biology and environment.
Can you get MS from a virus?
You can’t catch MS like a cold, but the Epstein-Barr virus (EBV)-which causes mononucleosis-is the strongest known trigger. People infected with EBV are 32 times more likely to develop MS. The virus doesn’t cause MS directly. Instead, it may confuse the immune system into attacking myelin because parts of the virus look similar to proteins in the nervous system. Nearly everyone with MS has had EBV, but most people who’ve had EBV never develop MS.
Does vitamin D help prevent or treat MS?
Low vitamin D levels are linked to a higher risk of developing MS, especially in regions far from the equator. People with serum levels below 50 nmol/L have a 60% higher risk. While taking vitamin D supplements won’t cure MS, maintaining levels above 75 nmol/L may reduce relapse rates and slow progression. Many neurologists recommend 2,000-5,000 IU daily, especially in winter months. It’s not a treatment, but it’s a proven supportive factor.
Can MS be cured?
There’s no cure for MS yet. But modern disease-modifying therapies can stop or significantly slow damage in most people. Some patients who start treatment early show no new lesions on MRI for over a decade. In rare cases, people with aggressive MS have had their immune systems reset through stem cell transplants, leading to long-term remission. Research into remyelination and immune tolerance is advancing fast-so while there’s no cure today, the path to one is clearer than ever.
Why do MS symptoms come and go?
In relapsing-remitting MS, symptoms flare up during active inflammation and improve when it calms down. This happens because the immune system attacks myelin in bursts. During a relapse, swelling and inflammation block nerve signals. When the attack ends, the swelling goes down, and nerves can sometimes reroute signals around damaged areas. But each attack leaves behind some permanent damage. Over time, these small losses add up, which is why some people eventually move into a progressive phase where symptoms steadily worsen.
Are MS treatments safe long-term?
Most disease-modifying therapies are safe for long-term use, but they require monitoring. Drugs like natalizumab carry a small risk of PML, so patients are tested for the JC virus before and during treatment. Others, like cladribine, temporarily lower white blood cell counts and need regular blood tests. The bigger risk isn’t the drug-it’s not treating the disease. Untreated MS leads to irreversible nerve damage. Doctors balance risks carefully, choosing treatments based on disease activity, patient age, and lifestyle.

swati Thounaojam
January 8, 2026 AT 12:31My aunt has MS and she just laughs when her legs go numb. Said it feels like her body’s playing tricks on her. She’s still gardening, though. Crazy strong woman.
Ken Porter
January 9, 2026 AT 20:52Why are we even spending billions on this? Just tell people to move to Arizona and take vitamin D. Problem solved.
Molly Silvernale
January 10, 2026 AT 19:20It’s not just an immune system malfunction-it’s a cosmic miscommunication. The body, in its infinite wisdom, mistakes the conductor of its symphony for an intruder. Myelin? That’s not insulation-it’s the sheet music. And now? The orchestra’s playing in the dark, and no one knows which note comes next.
And yet-we’re still here. Still feeling. Still thinking. Still trying to hear the music beneath the static.
What if the cure isn’t in suppressing the immune system-but in teaching it to listen again?
Not with drugs. Not with antibodies. But with silence. With stillness. With the kind of inner quiet that lets the body remember what it was meant to protect.
I don’t know if science can get there.
But I think the soul already did.
Joanna Brancewicz
January 11, 2026 AT 23:00IL-21 inhibition is showing promise in phase II trials for remyelination-especially in Pattern III lesions. The oligodendrocyte precursor cell (OPC) differentiation blockade is key. If we can modulate the microglial phenotype from M1 to M2, we might create a permissive niche for repair.
Also, sNfL is now a validated biomarker for subclinical disease activity. Thresholds >15 pg/mL correlate with 3x higher relapse risk within 12 months.
Evan Smith
January 13, 2026 AT 06:37So… we’re basically saying our immune system got confused because it watched too much sci-fi? ‘Oh no, myelin looks like a virus! Better destroy it!’
Also, why do all the cool drugs have names that sound like alien planets? Siponimod? Cladribine? Is this medicine or a Star Trek episode?
Luke Crump
January 13, 2026 AT 15:55They say the body attacks itself-but what if it’s not attacking? What if it’s screaming? What if MS isn’t a disease… but a protest? A cry from a system that’s been ignored for too long? We poison the earth, we numb our minds, we disconnect from nature-and then our own cells turn on us like betrayed lovers.
They give you pills. But they don’t give you silence. They don’t give you sunlight. They don’t give you the truth: maybe the cure isn’t in the lab-it’s in the forest.
Manish Kumar
January 15, 2026 AT 13:36Look, in India, we don’t have the luxury of fancy MRI scans and billion-dollar drugs. My cousin in Jaipur took ashwagandha, did yoga every morning, and drank warm turmeric milk. She’s been symptom-free for 8 years now. Western medicine is great, sure-but you can’t ignore the wisdom of centuries. Your body isn’t a machine to be fixed-it’s a river to be flowed with. Stop fighting it. Start listening. And maybe, just maybe, the myelin will come back on its own.
Also, why do Americans always think the answer is a new pill? We’ve been healing ourselves with herbs since the Vedas. You’re just catching up.
And yes, I know EBV is a trigger. But in rural India, 98% of people have EBV. Yet MS is rare. So maybe it’s not the virus. Maybe it’s the processed food. Maybe it’s the stress. Maybe it’s the fact that you’ve forgotten how to breathe.
Just saying.
Dave Old-Wolf
January 16, 2026 AT 02:23I’ve got a friend who’s been in remission for 12 years. She started treatment early, took her vitamin D, and walks 5 miles every day. No fancy supplements. Just consistency. It’s not magic-it’s discipline.
And honestly? The fatigue thing? It’s real. I thought I was just lazy until I saw how she’d nap for three hours after cooking dinner. It’s not laziness. It’s her body using every ounce of energy just to stay upright.
People don’t get that.
Prakash Sharma
January 17, 2026 AT 16:38Why are we letting foreign viruses dictate our health? Epstein-Barr? That’s a Western problem. We don’t have this in India because we don’t live like you do-overfed, overmedicated, and under-sun. Our ancestors didn’t need your drugs. They had clean air, clean food, and strong blood.
You want to cure MS? Stop importing diseases from other countries. Stop eating sugar. Stop being weak.
Donny Airlangga
January 17, 2026 AT 18:40My sister was diagnosed last year. She cried for three days. Then she started a blog. Now she helps other newly-diagnosed people navigate insurance, meds, and the emotional mess. She turned her pain into purpose.
It’s not about curing it. It’s about living with it-without letting it define you.
Kristina Felixita
January 19, 2026 AT 11:55My mom used to say: ‘The body remembers what the mind forgets.’ She had MS for 20 years, never took a single DMT-just sunshine, meditation, and chai with extra ginger. She passed last year, but she never let it take her joy.
And honestly? I think she was onto something.
Science is amazing, but it’s not everything.
Love? That’s the real treatment.
Lois Li
January 19, 2026 AT 14:30It’s wild how much we’ve learned in the last decade. The fact that we can now measure sNfL levels before symptoms show up? That’s huge. It means we can intervene before damage is done. That’s not just progress-it’s hope.
And the part about clemastine improving nerve speed? That’s the first real sign that repair is possible. Not suppression. Repair.
That’s the future.
christy lianto
January 21, 2026 AT 03:20My husband got diagnosed at 31. He’s 42 now. Still runs marathons. Still works full-time. Still makes pancakes on Sundays. MS didn’t end his life-it just changed the rules.
You don’t need to be cured to be unstoppable.