When you pick up a prescription, you might be handed a small white pill with a code on it - not the name you recognize from TV ads. That’s a generic drug. It works the same way as the brand-name version, costs a fraction of the price, and your insurance prefers it. But here’s the catch: not all generics are treated the same. And sometimes, you’ll still end up paying a lot more than you expected - even when a cheaper version exists.
How Insurance Decides What You Pay
Insurance companies don’t just randomly decide which drugs to cover. They use something called a formulary - a list of approved medications grouped into tiers. Think of it like a pricing ladder. The lower the tier, the less you pay.Generics almost always land on Tier 1. That means a 30-day supply might cost you $5 to $15. Brand-name drugs? They’re usually on Tier 2 or 3. Copays jump to $40, $60, even $100. Some plans don’t even use fixed copays - they charge you a percentage of the drug’s total cost, like 25% to 33%. That can mean hundreds of dollars for a single prescription.
Here’s why: generics don’t need to repeat expensive clinical trials. They just prove they’re chemically identical to the brand. That saves drugmakers money - and those savings get passed to insurers, who then pass them to you. In 2022, 90% of all prescriptions filled in the U.S. were generics. That’s $370 billion saved in one year alone.
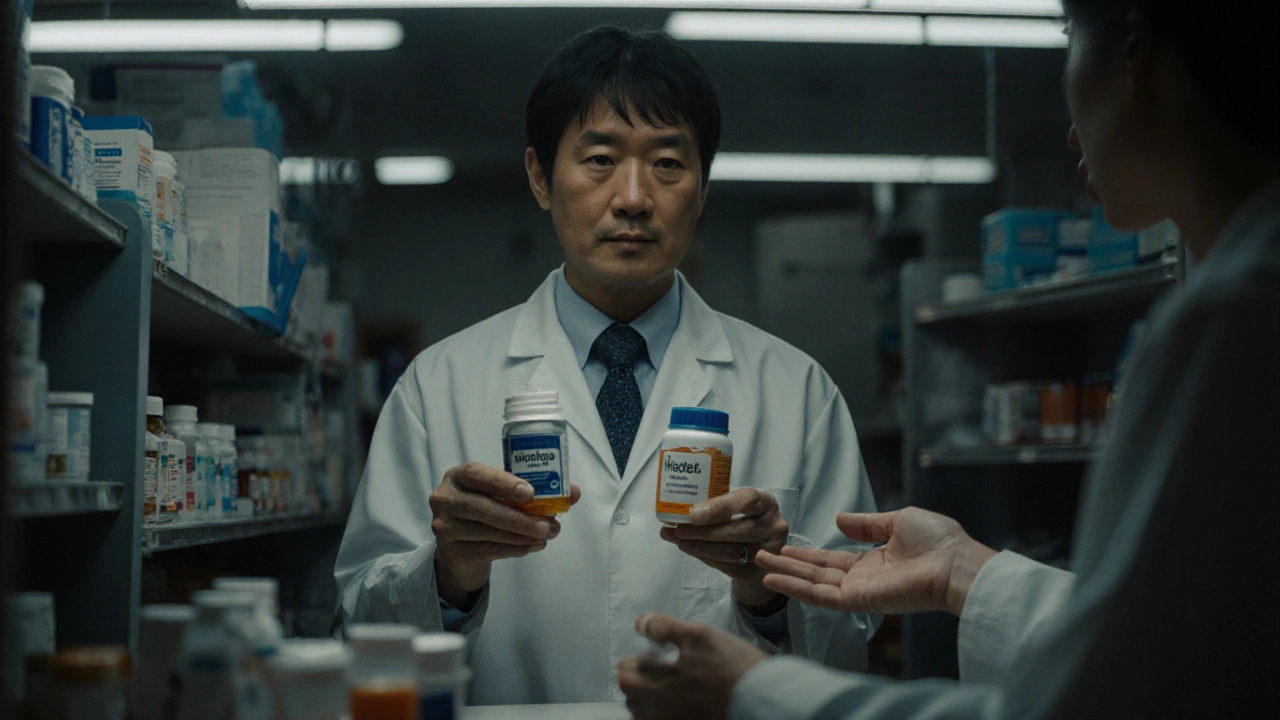
The Swap Rule: What Happens at the Pharmacy
When your doctor writes a prescription, they usually don’t specify whether it has to be brand or generic. That’s intentional. Most states allow pharmacists to automatically swap in a generic unless the doctor writes “dispense as written” or “no substitution.”But here’s where things get messy. If you walk in for your brand-name cholesterol pill - say, Crestor - and the pharmacist sees a generic rosuvastatin is available, they’ll give you the cheaper version. Your copay? $8. But if you insist on the brand, you don’t just pay the brand’s copay. You pay the generic copay plus the full price difference. So if Crestor costs $120 and the generic is $8, you pay $8 + $112 = $120. No discount. No mercy.
This isn’t a trick. It’s policy. Insurance wants you to choose the cheaper option. And they’ve built the system to make it financially painful not to.
When the System Won’t Let You Choose
Sometimes, even if you want the brand, your plan won’t let you get it - unless you jump through hoops.Many insurers use step therapy. That means you have to try the generic first. If it doesn’t work, you file a request. If it’s denied, you appeal. That process can take weeks. For someone with epilepsy, depression, or chronic pain, waiting isn’t just inconvenient - it’s dangerous.
Then there’s prior authorization. For brand-name drugs, 22.7% require this. For generics? Only 2.1%. That means if you need a brand, your doctor has to fill out paperwork, call the insurance company, maybe even fax in lab results. The average time to get approval? 3.2 business days. And 41% of those requests need a follow-up call.
Medicare Part D is especially strict. By law, pharmacists must substitute generics unless the doctor says otherwise. In 2022, 91% of Part D prescriptions were generics. If you’re on Medicare and your brand-name drug is replaced, you can’t just demand it back. You need a medical necessity exception - and not all states make that easy.
Medical Necessity: The Loophole That Isn’t Always a Loophole
There’s a way out: medical necessity. If you’ve tried two or three generics and they caused side effects, didn’t work, or made your condition worse, you can ask for the brand. But it’s not as simple as saying, “I don’t like it.”Insurance companies require documentation. In 67% of cases, your doctor must use a specific code - like YN1 - to justify the brand. Some states are stricter than others. California lets you switch back if a generic causes an adverse reaction. Texas only allows brands if no generic equivalent exists. And in 8 states, the bar is so high that patients give up.
Even then, some drugs are treated differently. For medications like levothyroxine (for thyroid), warfarin (a blood thinner), or phenytoin (for seizures), bioequivalence matters more. Small differences in inactive ingredients - like fillers or coatings - can affect how the drug is absorbed. That’s why 27 states have special rules for these drugs. They’re not just “equivalent.” They’re sensitive.
Why Some People Still Prefer the Brand
Let’s be honest: not everyone gets the same results with generics. A 2022 study in JAMA Neurology found that patients with epilepsy had 12.3% more seizures after switching from brand to generic. That’s not a small number. It’s life-changing.On forums like Reddit and Drugs.com, hundreds of people share stories: “My antidepressant stopped working after the switch.” “I had terrible headaches with the generic version of Lamictal.” “My thyroid levels went wild after the pharmacy changed my levothyroxine.”
The FDA says generics are identical in active ingredients, strength, and effectiveness. That’s true. But they don’t have to match the brand’s inactive ingredients - the dyes, binders, and coatings. For most people, that doesn’t matter. For others? It’s everything.
Dr. Aaron Kesselheim from Brigham and Women’s Hospital found that 68% of doctors have patients report different side effects with generics. That’s not because the drug doesn’t work. It’s because the body reacts to the whole pill - not just the active ingredient.
What You Can Do If You’re Struggling
If your insurance keeps pushing you toward a generic that doesn’t work:- Ask your doctor to write “dispense as written” on the prescription.
- Request a medical necessity exception. Keep records of side effects, lab results, and how you felt before and after the switch.
- Use GoodRx or SingleCare to compare cash prices. Sometimes, paying out of pocket is cheaper than your insurance copay.
- Check if the brand manufacturer offers a copay card. Many do - but Medicare and Medicaid patients can’t use them.
- Appeal. Most plans have a formal appeals process. Don’t give up after the first denial.
And if you’re on Medicare, use the Plan Finder tool. Compare plans before open enrollment. Some plans cover more brand-name drugs than others. Your current plan might not be the best fit.
The Bigger Picture: Savings vs. Safety
The system was built to save money. And it works. Generics save the U.S. healthcare system over $2 trillion every decade. They make medications accessible to millions who couldn’t otherwise afford them.But money-saving policies can’t ignore human biology. A pill that works for 9 out of 10 people might fail for the 11th. That’s not a flaw in the drug - it’s a flaw in the one-size-fits-all approach.
Policy makers are starting to notice. The FDA’s new labeling rules in 2025 will make therapeutic equivalence ratings clearer. Medicare is pushing to standardize prior authorization wait times to 72 hours. And some states are moving toward more patient-centered rules.
For now, the system favors generics. But it’s not broken - it just needs flexibility. You have the right to ask for what works. You just need to know how to ask.
What’s Next for Drug Coverage?
The landscape is changing. More new drugs are coming out as specialty medications - biologics, injectables, complex therapies. These rarely have generics. Instead, we’re seeing biosimilars, which are similar but not identical. Insurers are already starting to treat them differently.Also, brand companies are making their own generics - called “authorized generics.” These are made by the original manufacturer but sold under a different label. They often get better coverage than third-party generics because insurers trust them more.
And with the Inflation Reduction Act’s $2,000 out-of-pocket cap for Medicare Part D beneficiaries, people on expensive brand-name drugs are finally getting relief. That could shift how insurers design formularies in the coming years.
The future of drug coverage isn’t just about cost. It’s about matching the right drug to the right person - not the cheapest one on the shelf.
Why is my generic drug cheaper but my copay is still high?
Even if the generic is cheaper, your insurance plan may still charge a higher copay if the brand-name version is on a higher tier. You pay the copay for the tier your drug is on - not the actual price of the pill. If your plan requires you to pay the difference between brand and generic when you choose the brand, your out-of-pocket cost can be much higher than expected.
Can my pharmacist refuse to give me the brand-name drug?
No, they can’t refuse if your doctor wrote “dispense as written.” But if the prescription doesn’t specify that, most states allow pharmacists to substitute a generic unless you explicitly request the brand. Even then, you’ll likely pay more for the brand if a generic is available.
Do generics work the same as brand-name drugs?
Yes - for most people. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also be absorbed into the body at the same rate and to the same extent. But inactive ingredients can vary, and some patients report differences in side effects or effectiveness, especially with drugs like thyroid medication or seizure control drugs.
Why does my insurance make me try the generic first?
This is called step therapy. Insurers use it to control costs. They assume the generic will work for most people. If it doesn’t, you can appeal for the brand. But you’ll need documentation from your doctor showing the generic failed - and that process can take weeks.
Are there drugs where I should always avoid the generic?
For drugs with a narrow therapeutic index - like warfarin, levothyroxine, phenytoin, and some seizure meds - even small changes in absorption can be dangerous. Many doctors and patients prefer the brand for these. Some states have laws protecting access to the brand for these specific drugs. Always talk to your doctor before switching.
What’s the difference between a generic and an authorized generic?
A generic is made by a different company than the brand. An authorized generic is made by the original brand company but sold under a different label. Authorized generics are often chemically identical to the brand and may be covered more favorably by insurers because they’re seen as more reliable.
Can I use a copay card to lower the cost of a brand-name drug?
Yes - if you have commercial insurance. Many brand manufacturers offer copay cards that reduce your cost to $0-$10. But Medicare and Medicaid beneficiaries can’t use these cards. It’s illegal under federal law. If you’re on Medicare, you’ll need to rely on your plan’s formulary or appeal for coverage.

shubham seth
November 18, 2025 AT 13:46Yo so I got switched from Lipitor to some generic atorvastatin and my legs turned into jelly. Not metaphorical. Like, I couldn’t climb stairs without wheezing. Doc said 'it's the same molecule' - yeah, but my body ain’t a chemistry textbook. Now I pay cash with GoodRx. Worth every penny.
Kathryn Ware
November 20, 2025 AT 09:58As a pharmacist for 14 years, I see this daily 😔. People think generics are 'cheap knockoffs' - nope, they’re FDA-approved clones. BUT - the fillers? The dyes? The coating? Those can trigger allergies, GI issues, or even mood swings in sensitive folks. I’ve had patients cry because their anxiety meds 'stopped working' after a switch. It’s not placebo. It’s pharmacology. Always ask for the inactive ingredients list - most pharmacies will give it to you. And if your doc says 'dispense as written'? Honor it. No shame.
Also - authorized generics? Those are the OG brand made by the same factory, just repackaged. They’re often covered like generics but perform like brand. Ask your pharmacist if yours is one!
kora ortiz
November 21, 2025 AT 13:00Jeremy Hernandez
November 22, 2025 AT 23:04Let me guess - Big Pharma owns your insurance. They pay the insurance company to push generics so they can jack up brand prices later. And now they’re making 'authorized generics' - same factory, same pill, just a different label. That’s not capitalism. That’s a rigged game. The FDA? Totally bought. They let companies skip bioequivalence tests on the damn coatings. I’ve seen it. I’ve seen the emails. Don’t trust the system. Ever.
Tarryne Rolle
November 23, 2025 AT 03:57It’s not about the pill. It’s about control. We’ve outsourced our bodily autonomy to algorithms and insurance actuaries who’ve never held a human hand. We reduce medicine to cost-per-dose, then wonder why people feel broken. The real tragedy isn’t the generic - it’s that we accept this as normal. We’ve turned healing into a spreadsheet. And we call it progress.
Kyle Swatt
November 23, 2025 AT 07:12Look - I get it. I’ve been on levothyroxine for 12 years. Switched to generic once. My TSH went from 2.1 to 7.8. Felt like I was living underwater. Took me six months to get my doc to fight for the brand. The system doesn’t care until you’re dying. But here’s the thing - your body isn’t a robot. It remembers. It reacts. The FDA says 'bioequivalent' - but bio isn’t just chemistry. It’s biology. And biology is messy. If a pill makes you feel like trash, it doesn’t matter if it’s 'the same.' You’re not wrong. The system is.
Deb McLachlin
November 23, 2025 AT 10:42While the article presents a compelling overview of the current landscape, I would caution against conflating patient-reported outcomes with clinical efficacy. The JAMA Neurology study cited indicates an association, not causation. Moreover, the variability in individual response may be attributable to adherence, comorbidities, or concomitant medications. A controlled, double-blind crossover study would be necessary to isolate the effect of inactive ingredients. Until such evidence is robust, policy decisions should remain grounded in population-level data.
saurabh lamba
November 24, 2025 AT 05:07Kiran Mandavkar
November 24, 2025 AT 06:39Let’s be honest - the entire system is a charade. The FDA’s 'bioequivalence' standard is a joke. A 10% variation in absorption? That’s not equivalent - that’s gambling with someone’s life. And yet, we let corporations decide who lives and who suffers. Meanwhile, the same companies that make generics also own the brands. It’s not a free market. It’s a monopoly with a middleman. The real solution? Nationalize drug manufacturing. Or at least ban authorized generics. They’re just a loophole for price gouging dressed as innovation.
Eric Healy
November 24, 2025 AT 07:15Shannon Hale
November 25, 2025 AT 20:01OH MY GOD. I JUST GOT SWAPPED TO A GENERIC FOR MY ANTI-DEPRESSANT AND I FELT LIKE I WAS BEING DRAGGED THROUGH A HELLWIND FOR THREE WEEKS. I HAD NIGHTMARES. I CRIED IN THE SHOWER. I THOUGHT I WAS LOSING MY MIND. MY DOCTOR HAD TO FAX A 12-PAGE FORM JUST TO GET ME BACK ON THE BRAND. AND NOW THEY WANT TO SWITCH ME AGAIN NEXT MONTH. THIS IS TERRORISM. THIS IS NOT HEALTHCARE. THIS IS A CORPORATE TORTURE CHAMBER.
Holli Yancey
November 26, 2025 AT 06:41I just want to say thank you to everyone who’s shared their stories. I was scared to speak up because I thought I was being dramatic. But hearing others say 'me too' made me feel less alone. I’ve been on lamotrigine for 8 years. The generic made me feel like a ghost. I didn’t want to be alive. I didn’t want to be me. I fought for the brand. It took three appeals. But I’m here. And I’m okay. You’re not crazy. You’re not weak. You’re just human.
Gordon Mcdonough
November 27, 2025 AT 11:11Jessica Healey
November 29, 2025 AT 09:11Okay but like… I switched to generic levothyroxine and my hair started falling out. Like, clumps. I went from thick to see-through in 2 months. I cried. I Googled. I found 47 other people with the same thing. My doctor finally got me back on Synthroid. And now my hair’s growing back. So yeah - it’s not 'all in your head.' It’s in your follicles. And your thyroid. And your soul.
Levi Hobbs
November 30, 2025 AT 00:38Just a quick note - if you’re on Medicare and your brand-name drug is getting denied, ask about the 'Exception Request' form. It’s not hard. Just have your doctor write 'Medical Necessity: Patient experienced adverse reaction to two prior generics with documented lab abnormalities.' Include your TSH, INR, or seizure logs. Submit it with a cover letter. Most get approved on the second try. Don’t give up. And if you’re lucky, your plan might have a 'Preferred Generic' list - sometimes the authorized generic is on there. That’s your sweet spot.