Every year, millions of people turn to opioids for pain relief-after surgery, injury, or chronic conditions. But for many, what starts as a short-term solution becomes a dangerous long-term habit. In 2025, the risk isn’t just about addiction. It’s about overdose, suicide, and unnecessary suffering caused by poorly managed care. The good news? We now have clear, science-backed ways to reduce those risks without leaving people in pain.
Why Opioids Are Riskier Than You Think
Opioids aren’t the only tool for pain. They’re one of the last. And using them too early-or too long-can make things worse. The CDC found that patients taking more than 50 morphine milligram equivalents (MME) per day are nearly three times more likely to overdose than those on lower doses. That’s not a guess. It’s based on data from over 2 million patients between 2022 and 2024. The FDA updated opioid labels in July 2025 to reflect this. Now, every prescription bottle must state that 12.7% of patients on long-term opioid therapy develop moderate-to-severe opioid use disorder. That’s more than 1 in 8. And for every extra 20 MME above 50, the risk of overdose jumps by 1.7 times. This isn’t about scare tactics. It’s about numbers that doctors can’t ignore anymore. The goal isn’t to cut off pain relief-it’s to make sure opioids are used only when absolutely necessary, and only at the lowest dose possible.The New Rules for Prescribing Opioids
As of January 1, 2025, federal rules changed how opioids are prescribed. The CDC’s 2025 guidelines now say:- For acute pain (like after a dental procedure or sprained ankle), start with a three-day supply. Only extend to seven days if there’s clear, documented medical need.
- Avoid doses above 90 MME per day unless the patient has cancer, is in palliative care, or has been on that dose safely for years-with full documentation.
- Reassess the benefits and risks every time a patient hits 50 MME per day. That’s not a target. It’s a red flag.
What Works Better Than Opioids
The best way to reduce opioid risks is to avoid them in the first place. And there are proven alternatives.- NSAIDs like ibuprofen and naproxen are just as effective for most types of acute pain-and far safer. They’re growing in use at 6.1% per year.
- Acetaminophen, especially in combination with NSAIDs, reduces pain without the addiction risk.
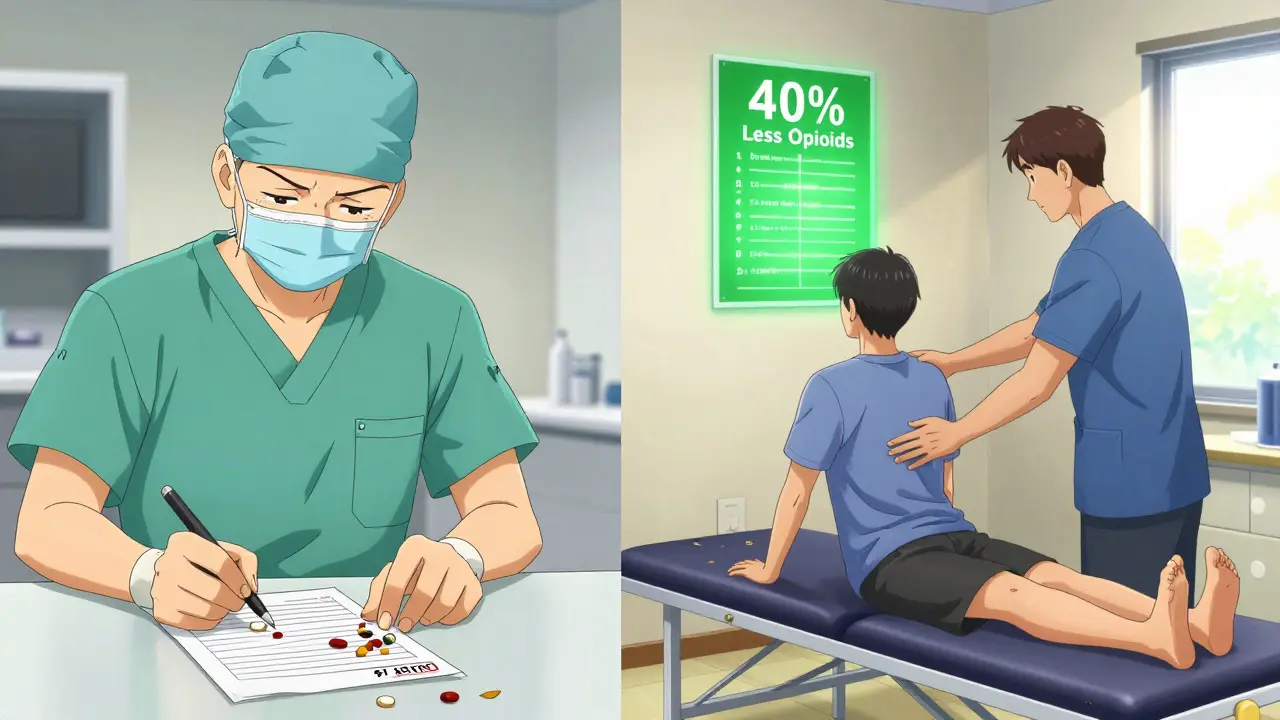
- Physical therapy helps with back pain, joint injuries, and post-surgery recovery. Studies show patients who start PT within a week of injury use 40% fewer opioids.
- Cognitive behavioral therapy (CBT) changes how the brain processes pain. It’s not a quick fix, but for chronic pain, it’s more effective long-term than opioids.
- CBD-based products are emerging as a non-addictive option. While still under study, early data shows promise for nerve pain and inflammation.
Who’s at Highest Risk?
Not everyone who takes opioids is at equal risk. Some people need them. Others need something else. The VA and CDC use simple screening tools to spot risk before prescribing:- Opioid Risk Tool (ORT): Scores patients based on personal or family history of substance use, mental health conditions, and age. A score above 8 means high risk-opioids should be avoided unless an addiction specialist is involved.
- Screener and Opioid Assessment for Patients with Pain (SOAPP): Used for chronic pain patients with complex histories, especially those with PTSD or depression.
What Happens When Opioids Are Stopped Too Fast
In the rush to cut back on opioids, some patients were abruptly taken off them. The result? A 23% spike in suicide attempts in 2024, according to a major study published in JAMA. The FDA now warns against rapid tapering. Sudden withdrawal can cause severe pain, anxiety, nausea, and even death in extreme cases. If a patient has been on opioids for months or years, reducing the dose must be slow-sometimes over months or even years. The key is communication. Patients need to be part of the decision. A 2025 survey by the U.S. Pain Foundation found that 7-10% of long-term users had their prescriptions cut without warning. Many ended up in emergency rooms because their pain returned worse than before.What Doctors Are Doing Right-and Wrong
Some doctors are adapting well. Dr. Michael Chen, a primary care doctor in Ohio, says his practice’s new three-day rule cut new cases of persistent opioid use by 35%. But he also had 12 patients show up in the ER because their pain wasn’t controlled. Others struggle with paperwork. Documentation for patients on over 50 MME now takes 27% longer to complete, according to a JAMA study. One doctor on Reddit said it added 2-3 extra hours a week just to fill out forms. The VA’s Opioid Safety Initiative (OSI) Toolkit helps. It includes checklists, PDMP checks, and integrated mental health support. Practices using it report better outcomes. But it takes training. The VA says it takes 8-12 weeks to fully train a team. Surgeons are lagging behind. Only 43% follow the 2025 CDC guidelines, compared to 82% of primary care doctors. Many still prescribe seven-day supplies after minor surgeries, even though research shows each extra day increases long-term use by 20%.
How to Stay Safe If You’re on Opioids
If you’re currently taking opioids for pain, here’s what you can do:- Ask your doctor: "Is this the lowest dose I can take?" and "Are there non-opioid options I haven’t tried?"
- Get your Prescription Drug Monitoring Program (PDMP) record checked regularly. It shows if you’re getting opioids from multiple doctors.
- Never mix opioids with alcohol, benzodiazepines, or sleep meds. That combination causes most fatal overdoses.
- Keep naloxone (Narcan) at home if you’re on doses over 50 MME. It can reverse an overdose in minutes.
- Track your pain levels daily. Use a simple scale from 1 to 10. If your pain isn’t improving after four weeks, ask for a plan B.
The Bigger Picture: What’s Changing in 2026
The opioid crisis isn’t solved. But progress is real. By 2027, 65% of acute pain cases are expected to be managed without opioids-up from 48% in 2025. The NIH is investing $125 million in new non-addictive pain treatments. States are expanding access to pain clinics. Telehealth for pain management is growing fast. But there’s still a shortage of 12,500 pain specialists in the U.S., especially in rural areas. Without them, even the best guidelines won’t help. The real win isn’t fewer prescriptions. It’s better care. Less suffering. Fewer deaths.Frequently Asked Questions
Are opioids ever safe for long-term pain?
Yes-but only in specific cases. Opioids can be appropriate for cancer pain, end-of-life care, or for patients who’ve tried everything else and still have severe pain. Even then, doses should stay below 50 MME per day, and patients need regular check-ins with their doctor. Long-term use outside these situations increases risk without proven benefit.
What should I do if my doctor wants to reduce my opioid dose?
Ask for a slow, personalized taper plan. Don’t agree to a rapid reduction. Request a timeline-ideally over months, not weeks. Ask for support like physical therapy or counseling during the process. If your doctor won’t work with you, seek a second opinion from a pain specialist.
Can I get pain relief without any medication?
Absolutely. Physical therapy, acupuncture, heat/cold therapy, mindfulness, and cognitive behavioral therapy (CBT) are all proven to reduce pain. Many people find that combining these with light movement-like walking or swimming-works better than pills. It takes time, but the results last longer.
Why do some doctors still prescribe opioids for seven days after surgery?
Because old habits die hard. Some surgeons still believe longer prescriptions prevent rebound pain. But research shows that’s not true. Most patients need opioids for only 3-5 days after minor surgery. The seven-day rule is outdated and increases the chance of leftover pills being misused or kept for later. The 2025 CDC guidelines say three days is enough for most cases.
Is naloxone really necessary if I’m not addicted?
Yes. Even people taking opioids exactly as prescribed can accidentally overdose-especially if they mix them with other meds, get sick, or change their dose. Naloxone is not for addicts. It’s for anyone on opioids. Keep it at home. Teach a family member how to use it. It’s simple, safe, and saves lives.


Nina Stacey
December 20, 2025 AT 12:31i just had knee surgery last month and was given 3 days of oxycodone like the new rules say and honestly it was enough
my pain was totally manageable with ibuprofen after that
they even gave me a free physical therapy session and i didn't even think to ask for it
why do people still think opioids are the only way? i mean seriously
Dominic Suyo
December 20, 2025 AT 17:48oh wow so now we’re criminalizing doctors who actually care about their patients? brilliant. because clearly the CDC has never met someone with chronic back pain who’s tried everything and still can’t get out of bed
let’s just hand out yoga mats and call it a day
the real crisis? bureaucrats who think pain is a lifestyle choice
and don’t even get me started on the 27% longer documentation time - that’s not safety, that’s bureaucratic gaslighting
Kevin Motta Top
December 22, 2025 AT 04:173-day rule works. i’ve seen it in ER. people come in with sprained ankles and leave with 3 pills and a PT referral. no drama. no stash. no addiction.
the system’s not perfect but it’s saving lives.
Alisa Silvia Bila
December 22, 2025 AT 14:12i think the biggest win here is that people are finally talking about alternatives instead of just reaching for pills
physical therapy changed my life after my rotator cuff injury
it wasn’t instant, but i didn’t end up dependent on something that could kill me
also, naloxone at home? yes. my brother keeps one in his glovebox. just in case.
Marsha Jentzsch
December 22, 2025 AT 18:35OH MY GOD I’M SO SICK OF THIS!!
my mom’s been on 60 MME for 12 years and now they’re gonna yank it away because some paper-pusher thinks it’s ‘too risky’??
she’s not an addict, she’s a survivor!!
you think she doesn’t know the risks?? she’s had 3 overdoses and still got up and went to work!!
why don’t you try living with 24/7 nerve pain and then tell me to ‘just do yoga’??
you people are monsters!!
Carolyn Benson
December 24, 2025 AT 01:16the real tragedy isn’t opioid use - it’s the commodification of suffering.
we’ve turned pain into a metric to be optimized, not a human experience to be honored.
if you reduce someone’s dose without addressing their trauma, you’re not healing - you’re just transferring the burden.
the body doesn’t lie, but the algorithm does.
and now we’re asking doctors to be data-entry clerks instead of healers.
what kind of society makes pain a compliance issue?
Chris porto
December 24, 2025 AT 16:16i get why people are scared. opioids feel like the only answer sometimes
but i’ve seen friends go from 120 MME to zero over 18 months with therapy and acupuncture
it was brutal, but they’re alive
and honestly? they sleep better now
the key is patience - and not treating people like numbers
Aadil Munshi
December 25, 2025 AT 04:14lol 38 states have limits but in india we just give out 30 pills like candy and call it ‘traditional pain management’
also, CBD? really? my uncle took it for arthritis and now he thinks he’s channeling chakras
but hey, at least he’s not overdosing
progress?
shivam seo
December 26, 2025 AT 00:11so now we’re importing american bureaucratic nonsense to the rest of the world? brilliant
we’ve got real problems like malaria and clean water and you’re worrying about whether someone gets 7 or 3 pills?
go fix your own healthcare system before preaching to the globe
also, naloxone? sounds like a drug company’s marketing ploy
benchidelle rivera
December 27, 2025 AT 14:59as a nurse who’s seen patients die from opioid overdose, i support every single guideline in this post.
the data is clear. the harm is real.
if you’re angry about reduced access, ask yourself: why did you need opioids in the first place?
and if you’re worried about tapering - that’s why we need pain specialists, not more prescriptions.
we owe it to our patients to do better.
Anna Sedervay
December 27, 2025 AT 20:32Have you considered that this entire ‘opioid crisis’ narrative is a pharmaceutical industry-driven psyop designed to shift public attention away from the real culprits: corporate greed, insurance denials, and the systemic erasure of holistic medicine?
They want you to believe that pills are the problem - when in reality, the system that makes pills the only affordable option is the true villain.
And don’t even get me started on how the VA’s ‘OSI Toolkit’ is just a Trojan horse for mandatory psychiatric evaluation.
They’re coming for your autonomy. Slowly. Methodically. With checklists.
Dev Sawner
December 28, 2025 AT 20:51It is a moral failure to prescribe opioids for non-cancer pain. The data is irrefutable. The CDC guidelines are not suggestions - they are ethical imperatives. To continue prescribing above 50 MME without multidisciplinary oversight is not medical practice - it is negligence. One must ask: who benefits from the continuation of this epidemic? The answer is not the patient. It is the system.
Moses Odumbe
December 30, 2025 AT 13:16just got my first naloxone kit from the pharmacy - free with insurance 😍
also got a coupon for 20% off CBD gummies
so now i’m basically a pain warrior with a kit and snacks
thanks CDC 🙌💊
bhushan telavane
January 1, 2026 AT 10:42in my village in india, we use turmeric paste and massage for back pain. no pills. no doctors. just family.
maybe the answer isn’t more rules - but more connection.
Nina Stacey
January 3, 2026 AT 10:07to the person who said their mom’s been on 60 MME for 12 years - i’m so sorry you’re going through that
i don’t know your story but i hear you
maybe the answer isn’t cutting off the meds but building better support - like home visits, therapy, pain coaches
we can care about safety and still care about people
just saying