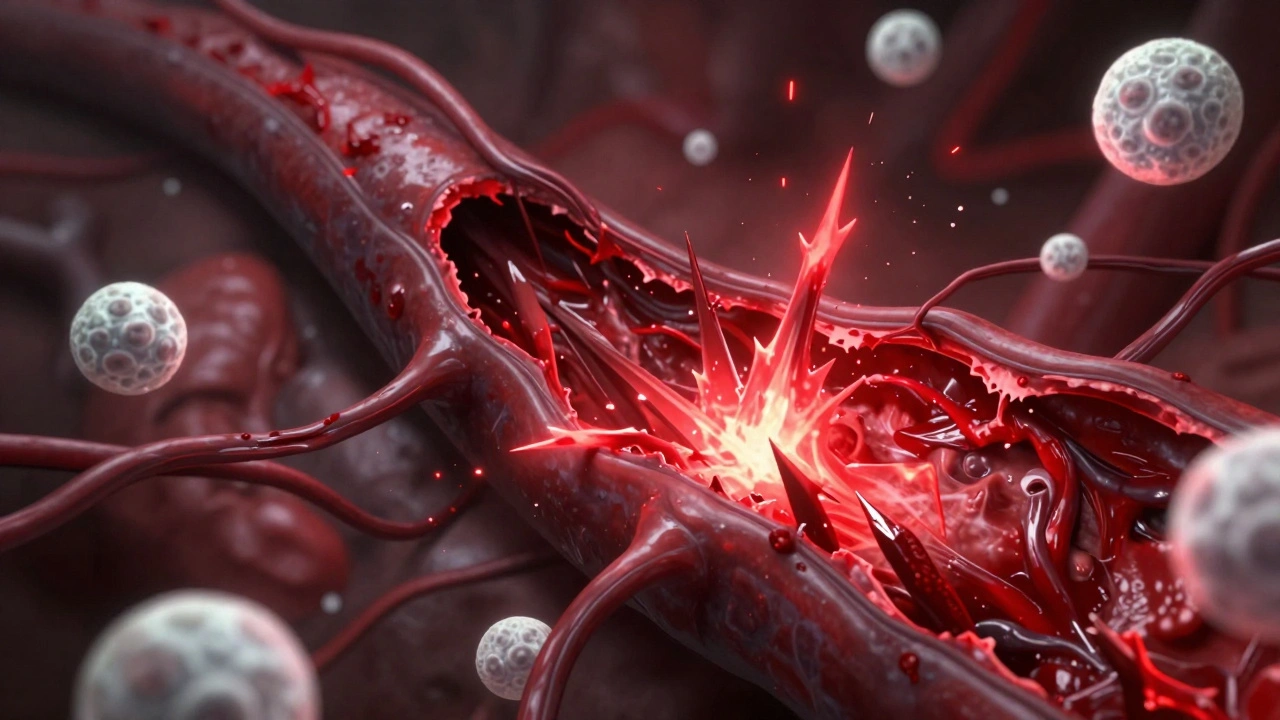
When your immune system turns on your own blood vessels, things get dangerous fast. Vasculitis isn’t just a buzzword-it’s a real, often hidden condition where your body attacks the very tubes that carry blood to your organs. This isn’t a simple rash or a bad cold. It’s inflammation tearing through arteries, veins, and capillaries, starving tissues of oxygen, and sometimes causing strokes, kidney failure, or heart attacks. And it’s more common than most people realize.
What Exactly Happens When Vasculitis Strikes?
Your blood vessels are like highways for oxygen and nutrients. In vasculitis, your immune system mistakes the walls of these vessels for invaders. White blood cells swarm in, causing swelling, thickening, and eventually damage. The vessel can narrow, block completely, or even bulge into a dangerous aneurysm. This isn’t guesswork-it’s a documented process. Histology shows immune cells breaking down the middle layer of arteries, destroying the internal elastic lamina, which normally keeps vessels strong and flexible. Once that’s gone, aneurysms form. That’s why early diagnosis matters so much.It’s Not One Disease-It’s a Family of Disorders
Vasculitis isn’t a single condition. It’s grouped by the size of the blood vessels it targets. That distinction changes everything-from symptoms to treatment.- Large-vessel vasculitis hits the aorta and its big branches. Giant cell arteritis (GCA) is the most common here, usually affecting people over 50. It often starts with scalp tenderness, jaw pain when chewing, and sudden vision loss. Takayasu arteritis, rarer and often seen in younger women, can cause weak pulses in the arms and high blood pressure.
- Medium-vessel vasculitis includes polyarteritis nodosa and Kawasaki disease. Kawasaki disease mostly affects kids under 5. If untreated, up to 25% develop coronary artery aneurysms-something that can lead to heart attacks in children.
- Small-vessel vasculitis is the most dangerous because it hits organs silently. ANCA-associated vasculitis includes granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA). These can attack kidneys, lungs, and nerves without warning. You might think you have the flu, but your kidneys are already failing.
How Do Doctors Diagnose It?
There’s no single blood test for vasculitis. Diagnosis is like putting together a puzzle. Doctors look at four things: your symptoms, lab results, imaging, and biopsy.- Symptoms vary wildly. Skin: purple spots, ulcers, or hives. Lungs: coughing blood or shortness of breath. Kidneys: foamy urine or swelling in legs. Nerves: numbness in hands or feet. Joint pain. Fatigue. Fever. These mimic everything from the flu to arthritis.
- Lab tests show inflammation: ESR over 50 mm/hr, CRP above 5 mg/dL. But the real clue is ANCA-anti-neutrophil cytoplasmic antibodies. c-ANCA targeting proteinase-3 is 80-90% specific for GPA. p-ANCA often points to MPA.
- Imaging like CT angiography or PET scans can show vessel wall thickening or blockages. In GCA, ultrasound of the temporal artery often shows a "halo sign"-a dark ring around the artery from swelling.
- Biopsy is the gold standard. A small piece of affected tissue-skin, kidney, nerve, or temporal artery-under the microscope shows immune cells eating through vessel walls. Leukocytoclastic vasculitis? That’s the classic sign in skin biopsies: nuclear debris scattered around tiny vessels.
Here’s the catch: most people wait 6 to 12 months before getting diagnosed. Symptoms start small. A sore throat. Aching joints. A rash. Doctors think it’s allergies or a virus. By the time they suspect vasculitis, damage may already be done.

What Are the Treatment Options Today?
Treatment depends on severity and which vessels are involved. But the goal is always the same: stop the immune system from attacking, then keep it stopped.- High-dose steroids like prednisone are the first line. You might start at 0.5-1 mg per kg of body weight daily. That’s a lot-think 50-100 mg a day. It works fast to calm inflammation.
- Immunosuppressants follow. Cyclophosphamide was the standard for decades. Now, rituximab is often preferred-it targets B cells that drive the attack. For GPA and MPA, studies show rituximab is just as effective as cyclophosphamide, with fewer long-term side effects like cancer risk.
- Avacopan is the newest player. Approved by the FDA in 2021, it blocks a protein called C5a that pulls immune cells into vessels. In the ADVOCATE trial, patients on avacopan had 2,000 mg less total steroid exposure over a year. That means fewer moon face, bone loss, and diabetes risks.
- Tocilizumab is now approved for giant cell arteritis. It blocks interleukin-6, a key inflammation driver. Patients can reduce steroid doses faster and still stay in remission.
- For Kawasaki disease, high-dose IVIG (intravenous immunoglobulin) and aspirin are standard. Early treatment cuts aneurysm risk from 25% to under 5%.
- Buerger’s disease? No drugs help if you keep smoking. Quitting is the only cure.
After the first 3-6 months of aggressive treatment, most patients switch to maintenance drugs: azathioprine, methotrexate, or rituximab every 6 months. Treatment lasts 18-24 months minimum. Some need it longer.
What’s the Prognosis? Can You Survive It?
The good news: most people go into remission. About 80-90% of those with ANCA-associated vasculitis do. The bad news: half of them relapse within five years. That’s why monitoring doesn’t stop after treatment ends.The Five Factor Score helps predict survival in polyarteritis nodosa. If you have no major organ damage (kidney, heart, GI), your 5-year survival is 95%. If you have two or more, it drops to 50%. That’s why catching kidney involvement early is critical-many patients have no symptoms until their creatinine spikes.
For giant cell arteritis, vision loss can be permanent if treatment is delayed even a few days. That’s why doctors treat suspected GCA immediately, even before biopsy results come back.

What’s New in Research?
Science is moving fast. The Vasculitis Clinical Research Consortium is testing new biomarkers like BAFF and urinary MCP-1 to predict flares before symptoms show. That could mean catching relapses early-before organs get damaged.Mepolizumab, a drug used for severe asthma, is showing promise in EGPA. In early trials, it cut relapse rates by half. Abatacept, which blocks T-cell activation, is being tested for GCA. And gene studies are starting to uncover why some people develop vasculitis and others don’t.
What Should You Do If You Suspect Vasculitis?
If you have unexplained symptoms like:- Purple skin spots that don’t fade when pressed
- Joint pain with no injury
- Coughing blood
- Numbness or weakness in limbs
- Severe headaches with jaw pain or vision changes
Don’t wait. See a rheumatologist. Primary care doctors often miss this. You need someone who knows the patterns. Urine tests, kidney function checks, and ANCA blood tests should be done-even if you feel "just tired."
Early treatment saves organs. Late treatment saves lives. But it’s often too late by then.

Ashley Skipp
December 13, 2025 AT 04:58My cousin had this and they almost lost her kidney before anyone figured it out
Donna Anderson
December 13, 2025 AT 11:39OMG this is so important!! I had weird rashes and numb hands for months and everyone thought it was stress until my rheum doc spotted the ANCA pattern. I’m alive because I pushed for bloodwork. Don’t ignore weird symptoms!! 🙌
sandeep sanigarapu
December 14, 2025 AT 02:16It is a serious condition. Many cases go undiagnosed due to lack of awareness. Early detection saves lives. Medical professionals must be trained to recognize the subtle signs. Public education is essential.
Robert Webb
December 14, 2025 AT 10:45I’ve been reading up on this because my mom was diagnosed with GCA last year-she went blind in one eye for three days before the steroids kicked in. The part about treating it before biopsy results is terrifying but makes total sense. I didn’t realize how fast this can escalate. It’s like your body is literally trying to cut off your own oxygen supply. And the fact that avacopan cuts steroid exposure by 2000mg over a year? That’s a game-changer for quality of life. No more moon face, no more osteoporosis creeping in while you’re trying to survive. I wish more doctors talked about this stuff in plain terms.
Rob Purvis
December 14, 2025 AT 15:59Wait-so p-ANCA is linked to MPA, and c-ANCA to GPA? And the halo sign on ultrasound is basically a red flag for GCA? I’ve been seeing these terms all over my mom’s medical records and never connected them. This is the clearest breakdown I’ve ever read. Also, the fact that Kawasaki can cause heart attacks in toddlers? That’s horrifying. I’m going to print this out and give it to my pediatrician.
Laura Weemering
December 16, 2025 AT 14:03...and yet, Big Pharma is quietly funding these "new treatments" while hiding the real cause: glyphosate in our food, 5G radiation, and the CDC’s suppression of autoimmune research. They don’t want you to know vasculitis is triggered by environmental toxins-because then people would stop buying processed food and start demanding clean water. The FDA approved avacopan? Funny how that lines up with the patent expiration of prednisone...
Audrey Crothers
December 16, 2025 AT 16:48THIS. I had EGPA and mepolizumab saved my life. I was wheezing and coughing blood-I thought I had asthma. Turns out, my eosinophils were on a rampage. Now I get the shot every 4 weeks and I can breathe again. 🤍 If you have unexplained asthma + rashes + fatigue, ask for ANCA and eosinophil count. Don’t wait. I almost didn’t make it.
Stacy Foster
December 16, 2025 AT 17:40They’re lying about the treatment timeline. You don’t need 18 months of immunosuppressants-you need detox, alkaline diet, and magnesium. The whole system is rigged to keep you on drugs forever. My cousin got cured with turmeric and fasting. Why won’t they tell you that?
Lawrence Armstrong
December 17, 2025 AT 00:07My dad had GPA. He’s been in remission for 7 years now. Rituximab was a miracle-no more chemo, no more hospital stays. I’m just glad we found it before his lungs gave out. 🙏
nikki yamashita
December 18, 2025 AT 12:05Just got my ANCA results back-positive for p-ANCA. I’m scared but also relieved. At least now I know what’s going on. Thanks for sharing this, it helped me ask the right questions.
Nathan Fatal
December 18, 2025 AT 18:01What fascinates me is how the immune system-designed to protect-becomes the architect of its own destruction. Vasculitis isn’t just a disease; it’s a mirror reflecting the fragility of biological trust. We evolved to defend against pathogens, yet here we are, attacking the very infrastructure that sustains us. The irony is profound. And yet, medicine now offers tools to retrain this betrayal. That’s not just science-it’s redemption.
Levi Cooper
December 20, 2025 AT 05:10Why are we even treating this with drugs? In my country, we just use traditional herbs and acupuncture. America’s obsession with pills is why people keep getting sicker. This whole system is broken.
Reshma Sinha
December 21, 2025 AT 16:57As a medical researcher in India, I’ve seen multiple cases of ANCA-associated vasculitis in young adults with no prior history. The diagnostic delay is alarming-often over 9 months. We’re now using urinary MCP-1 as a surrogate marker in resource-limited settings. It’s not perfect, but it’s better than waiting for organ failure. Early intervention saves kidneys, and kidneys save lives.